Tracheotomy
Definition
A tracheotomy is a surgical procedure that opens up the windpipe (trachea). It is performed in emergency situations, in the operating room , or at bedside of critically ill patients. The term tracheostomy is sometimes used interchangeably with tracheotomy. Strictly speaking, however, tracheostomy usually refers to the opening itself while a tracheotomy is the actual operation.
Purpose
A tracheotomy is performed if enough air is not getting to the lungs, if the person cannot breathe without help, or is having problems with mucus and other secretions getting into the windpipe because of difficulty swallowing. There are many reasons why air cannot get to the lungs. The windpipe may be blocked by a swelling; by a severe injury to the neck, nose, or mouth; by a large foreign object; by paralysis of the throat muscles; or by a tumor. The patient may be in a coma, or need a ventilator to pump air into the lungs for a long period of time.
Demographics
Emergency tracheotomies are performed as needed in any person requiring one.
Description
Emergency tracheotomy
There are two different procedures that are called tracheotomies. The first is done only in emergency situations and can be performed quite rapidly. The emergency room physician or surgeon makes a cut in a thin part of the voice box (larynx) called the cricothyroid membrane. A tube is inserted and connected to an oxygen bag. This emergency procedure is sometimes called a cricothyroidotomy .
Surgical tracheotomy
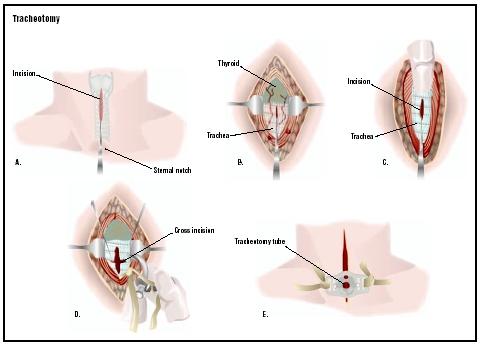
The second type of tracheotomy takes more time and is usually done in an operating room. The surgeon first makes a cut (incision) in the skin of the neck that lies over the trachea. This incision is in the lower part of the neck between the Adam's apple and top of the breastbone. The neck muscles are separated and the thyroid gland, which overlies the trachea, is usually cut down the middle. The surgeon identifies the rings of cartilage that make up the trachea and cuts into the tough walls. A metal or plastic tube, called a tracheotomy tube, is inserted through the opening. This tube acts like a windpipe and allows the person to breathe. Oxygen or a mechanical ventilator may be hooked up to the tube to bring oxygen to the lungs. A dressing is placed around the opening. Tape or stitches (sutures) are used to hold the tube in place.
After a nonemergency tracheotomy, the patient usually stays in the hospital for three to five days, unless there is a complicating condition. It takes about two weeks to recover fully from the surgery.
Diagnosis/Preparation
Emergency tracheotomy
In the emergency tracheotomy, there is no time to explain the procedure or the need for it to the patient. The patient is placed on his or her back with face upward (supine), with a rolled-up towel between the shoulders. This positioning of the patient makes it easier for the doctor to feel and see the structures in the throat. A local anesthetic is injected across the cricothyroid membrane.
Nonemergency tracheotomy
In a nonemergency tracheotomy, there is time for the doctor to discuss the surgery with the patient, to explain what will happen and why it is needed. The patient
Aftercare
Postoperative care
A chest x ray is often taken, especially in children, to check whether the tube has become displaced or if complications have occurred. The doctor may prescribe antibiotics to reduce the risk of infection. If the patient can breathe without a ventilator, the room is humidified; otherwise, if the tracheotomy tube is to remain in place, the air entering the tube from a ventilator is humidified. During the hospital stay, the patient and his or her family members will learn how to care for the tracheotomy tube, including suctioning and clearing it. Secretions are removed by passing a smaller tube (catheter) into the tracheotomy tube.
It takes most patients several days to adjust to breathing through the tracheotomy tube. At first, it will be hard even to make sounds. If the tube allows some air to escape and pass over the vocal cords, then the patient may be able to speak by holding a finger over the tube. Special tracheostomy tubes are also available that facilitate speech.
The tube will be removed if the tracheotomy is temporary. Then the wound will heal quickly and only a small scar may remain. If the tracheotomy is permanent, the hole stays open and, if it is no longer needed, it will be surgically closed.
Home care
After the patient is discharged, he or she will need help at home to manage the tracheotomy tube. Warm compresses can be used to relieve pain at the incision site. The patient is advised to keep the area dry. It is recommended that the patient wear a loose scarf over the opening when going outside. He or she should also avoid contact with water, food particles, and powdery substances that could enter the opening and cause serious breathing problems. The doctor may prescribe pain medication and antibiotics to minimize the risk of infections. If the tube is to be kept in place permanently, the patient can be referred to a speech therapist in order to learn to speak with the tube in place. The tracheotomy tube may be replaced four to 10 days after surgery.
Patients are encouraged to go about most of their normal activities once they leave the hospital. Vigorous activity is restricted for about six weeks. If the tracheotomy is permanent, further surgery may be needed to widen the opening, which narrows with time.
Risks
Immediate risks
There are several short-term risks associated with tracheotomies. Severe bleeding is one possible complication. The voice box or esophagus may be damaged during surgery. Air may become trapped in the surrounding tissues or the lung may collapse. The tracheotomy tube can be blocked by blood clots, mucus, or the pressure of the airway walls. Blockages can be prevented by suctioning, humidifying the air, and selecting the appropriate tracheotomy tube. Serious infections are rare.
Long-term risks
Over time, other complications may develop following a tracheotomy. The windpipe itself may become damaged for a number of reasons, including pressure from the tube, infectious bacteria that forms scar tissue, or friction from a tube that moves too much. Sometimes the opening does not close on its own after the tube is removed. This risk is higher in tracheotomies with tubes remaining in place for 16 weeks or longer. In these cases, the wound is surgically closed. Increased secretions may occur in patients with tracheostomies, which require more frequent suctioning.
High-risk groups
The risks associated with tracheotomies are higher in the following groups of patients:
- children, especially newborns and infants
- smokers
- alcoholics
- obese adults
- persons over 60
- persons with chronic diseases or respiratory infections
- persons taking muscle relaxants , sleeping medications, tranquilizers, or cortisone
Normal results
Normal results include uncomplicated healing of the incision and successful maintenance of long-term tube placement.
Morbidity and mortality rates
The overall risk of death from a tracheotomy is less than 5%.
Alternatives
For most patients, there is no alternative to emergency tracheotomy. Some patients with pre-existing neuromuscular disease (such as ALS or muscular dystrophy) can be sucessfully managed with emergency noninvasive ventilation via a face mask, rather than with tracheotomy. Patients who receive nonemergency tracheotomy in preparation for mechanical ventilation may often be managed instead with noninvasive ventilation, with proper planning and education on the part of the patient, caregiver, and medical staff.
Resources
books
Bach, John R. Noninvasive Mechanical Ventilation. NJ: Hanley and Belfus, 2002.
Fagan, Johannes J., et al. Tracheotomy. Alexandria, VA: American Academy of Otolaryngology-Head and Neck Surgery Foundation, Inc., 1997.
"Neck Surgery." In The Surgery Book: An Illustrated Guide to 73 of the Most Common Operations , ed. Robert M. Younson, et al. New York: St. Martin's Press, 1993.
Schantz, Nancy V. "Emergency Cricothyroidotomy and Tracheostomy." In Procedures for the Primary Care Physician , ed. John Pfenninger and Grant Fowler. New York: Mosby, 1994.
other
"Answers to Common Otolaryngology Health Care Questions." Department of Otolaryngology–Head and Neck Surgery Page. University of Washington School of Medicine [cited July 1, 2003]. http://weber.u.washington.edu/~otoweb/trach.html .
Sicard, Michael W. "Complications of Tracheotomy." The Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences. December 1, 1994 [cited July 1, 2003]. http://http:www.bcm.tmc.edu/oto/grand/12194.html .
Jeanine Barone, Physiologist Richard Robinson
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Tracheotomy is performed by a surgeon in a hospital.
QUESTIONS TO ASK THE DOCTOR
- How do I take care of my trachesotomy?
- How many of your patients use noninvasive ventilation?
- Am I a candidate for noninvasive ventilation?
Carmen
My dad is 93 yrs old and has been on a ventilator for over a week.
It had a colasped lung, pneumonia, and the sack around the lung had two different infections. They have a tube in his chest to drain the infection. Now they want to put him on a trech. He is normally in good health and very active. What are his chances of just being on the trech temporally?
My complaints were; trouble breathing, acid reflux, belly pains, mucus and other secretions entering windpipe, windpipe 1/2 blocked off, Insomnia, not able to feed, constant throwing up, not being able to go #1 and #2 without pain, painful to talk, painful to breath/swallow, painful to concentrate on people talking to me directly, and last but not least a constant cough while spitting up black saliva from time to time with the cough.
I have lymph nodes in my neck that are enlarged and feels like huge soft pebbles in which you may move them around the asophogus freely within the neck. At first they said they were thyroids but when I continued to go back in the E.R. they mentioned that the thyroids were not swollen. They can not find out exactly wat is wrong with me in the E.R. I personally believe I have a tumor in my neck but will not find out until tomorrow when administered the Gastro Intestinal Camera.
I have infections in my belly that cause acid to shoot up in my throat. The anti-biotics they prescribed to me are, 20 PANTOPRAZOLE ER 40MG (Generic for fluid Protonix) which was injected in me by an I.V. Another one was PRILOSEC 20MG. They also prescribed me PROAIR HFA (Albuterol Sulfate) Inhalation Aerosol for Oral Inhalation.
I am looking for someone that has similar problems that may contact me with information about these symptoms and might be able to give me a little heads up. More than anything, I am scared and frightened that my life is in jeopardy. My family are not supportive and do not care. If their is a person out there that I may relate to, please contact me via email. IMike27I@hotmail.com
My husband had a trach done after a motorcycle accident . It was in place to help him breaath with a vent. he was taken off the vent and the trach was taken out after about a month. This has been 2 years ago. He is having problem every now and then where he seems to not be able to get any air in or out. This sometimes happens at night. Very scary it has also happened while he has been eating. It take several seconds which seems like minutes to get air moving again. I was just wondering if there could be scar tissue there from the trach that could cause this problem.
here is the info on the procedure that will be done
i am very much worried but hav hope and trust in GOD.
Normally for a patient like her, how many days takes to recover completely.
she is 53 years of age.
Now My brother taking care of daily cleaning , Now my father wants to close the hole is there any chance to do that
whya tube so soon?
Wendy
75- no if he comes off the vent he will die. survival chance is 0% 69- As his lung heals (He may have a chest tube if its badly collaped- They will slowly wean him off until he can become off the vent. There is no other way- him fighting it is good- he needs to be semi-conscious to be able to breathe on his own although its hard to watch. 68- The nurses WILL NEVER remove the trach unless a doctor orders it.
Again people this isn't medical advice- and you need to talk to your doctors more- and even your nurses. ALso this procedure is VERY RISKY don't ever do this really because you could hit the arteries and kill the poor person. Try the Heimlich EFFECTIVELY and then CPR and sometimes CPR makes the food come out. (chest compressions can push it out).
He was told that a device could be inserted to help his vocal cords open and close properly.
Is this a safe procedure? He is in the mid 70's and uses his voice a lot in speaking. We were told a couple months ago, that there were two polyps that needed to be removed and that the trache would be in permanantly. We were so disappointed because we had been told that a year from when he had stints inserted in his heart that this device could be inserted.
Help!!! He is so tired of the trache, but we're blessed that he is still alive.
Please comment
I wonder if there is any suggestions for us to communicate with him.
He is trying to talk to us but we can't understand. He is able to close his eyes so I'm only able to ask him questions where he can answer for Yes or No.
We live in South America. Any suggestion will help!! Thank u and I'm sorry for my grammar / spelling.
i want to know if it is possible for her to do her home ventilation care at home---instead of at a nursing home.
i admit i dont really know much about this subject--but greatly appreciate any info...
Thank you for your time and effort
we consulted few doctors where they differ in opinion. One of the doctor want me to go for immediate CO2 laser treatment , where he will try to open up the airway. He said end result may be opening of 6-9mm and it will be just a day care procedure.
But other doctors are asking us to wait for atleast 6 weeks in a hope that vocal cords may start moving by which I will have a better airway and surgery will be less complicated. they are even saying its ok to wait for 3 months before any surgical intervention.
R we going wrong anywhere?