Parathyroidectomy
Definition
Parathyroidectomy is the removal of one or more parathyroid glands. A person usually has four parathyroid glands, although the exact number may vary from three to seven. The glands are located in the neck, in front of the Adam's apple, and are closely linked to the thyroid gland. The parathyroid glands regulate the balance of calcium in the body.
Purpose
Parathyroidectomy is usually performed to treat hyperparathyroidism (abnormal over-functioning of the parathyroid glands).
Demographics
The number of parathyroidectomy procedures has risen due to routine measurement of calcium in the blood. Incidence rates vary between 25 and 50 per 100,000 persons. The number of procedures in females is approximately twice that of males. The incidence of parathyroidectomy rises after age 40.
Description
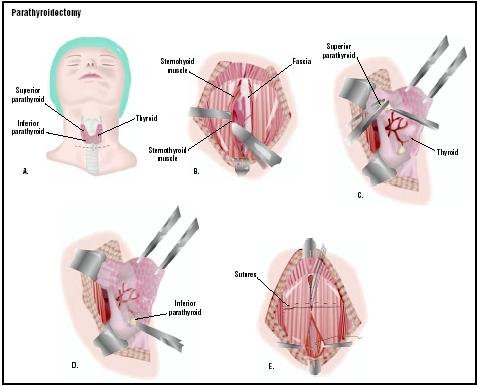
The operation begins when an anesthesiologist administers general anesthesia. The surgeon makes an incision in the front of the neck where a tight-fitting necklace would rest. All of the parathyroid glands are identified. The surgeon then identifies the diseased gland or glands, and confirms the diagnosis by sending a piece of the gland(s) to the pathology department for immediate microscopic examination. The diseased glands are then removed, and the incision is closed and covered with a dressing.
Parathyroidectomy patients usually stay overnight in the hospital after the operation. Some patients remain hospitalized for one or two additional days.
Diagnosis/Preparation
Prior to the operation, the diagnosis of hyperparathyroidism should be confirmed using lab tests. Occasionally, physicians order computed tomography scans ( CT scans ), ultrasound exams, or magnetic resonance imaging (MRI) tests to determine the total number of parathyroid glands, and their location prior to the procedure.
Parathyroidectomy should only be performed when other non-operative methods have failed to control a person's hyperparathyroidism.
Preparation is similar to other surgical procedures requiring general anesthetic. The patient is not allowed any food or drink by mouth after midnight the night before surgery. He or she should ask the physician for specific directions regarding preparation for surgery, including food, drink, and medication intake.
Aftercare
The incision should be watched for signs of infection. In general, no special wound care is required.
The calcium level is monitored during the first 48 hours after the operation by obtaining frequent blood samples for laboratory analysis.
Most individuals require only two or three days of hospitalization to recover from the operation. They can usually resume most of their normal activities within one to two weeks.
Risks
The major risk of parathyroidectomy is injury to the recurrent laryngeal nerve (a nerve that lies very near the parathyroid glands and serves the larynx or voice box). If this nerve is injured, the voice may become hoarse or weak.
Occasionally, too much parathyroid tissue is removed, and a person may develop hypoparathyroidism (under-functioning of the parathyroid glands). If this occurs, he or she will require daily calcium supplements.
In some cases, the surgeon is unable to locate all of the parathyroid glands, and cannot remove them in one procedure. A fifth or sixth gland may be located in an aberrant place such as the chest (ectopic parathyroid). If this occurs, the hyperparathyroidism may not be corrected with one operation, and a second procedure may be required to find all of the patient's remaining parathyroid gland tissue.
Normal results
The surgery progresses normally if the diseased parathyroid glands are located and removed from the neck region.
Morbidity and mortality rates
Hematoma formation (collection of blood under the incision) is a possible complication of any operative procedure. However, in procedures that involve the neck it is of particular concern because a rapidly enlarging hematoma can obstruct the airway.
Infection of the surgical incision may occur, as it may in any operative procedure, but this is uncommon in parathyroidectomy.
Before the function of the parathyroid gland was understood, people undergoing a thyroidectomy often died due to the lack of calcium in their blood caused by removal of the parathyroid glands. This is not a problem today.
Alternatives
There is no safe or reliable alternative to removal of the parathyroid glands for the treatment of hyperparathyroidism. Oral phosphates can lower serum calcium levels, but the long-term use of this approach is not well understood.
See also Thyroidectomy .
Resources
books
Bilezikan, J.P., R. Marcus, M. Levine. The Parathyroids 2nd Edition. St. Louis: Academic Press, 2001.
Bland, K.I, W.G. Cioffi, M.G. Sarr. Practice of General Surgery. Philadelphia: Saunders, 2001.
Randolph, G. Surgery of Thyroid and Parathyroid Glands. St. Louis: Elsevier, 2002.
Schwartz, S.I., J.E. Fischer, F.C. Spencer, G.T. Shires, J.M. Daly. Principles of Surgery 7th edition. New York: McGraw Hill, 1998.
Townsend C., K.L. Mattox, R.D. Beauchamp, B.M. Evers, D.C. Sabiston Sabiston Review of Surgery 3rd Edition. Philadelphia: Saunders, 2001.
periodicals
Awad, S.S., J. Miskulin, N. Thompson. "Parathyroid Adenomas versus Four-gland Hyperplasia as the Cause of Primary Hyperparathyroidism in Patients with Prolonged Lithium Therapy." World Journal of Surgery 27, no.4 (2003): 486-8.
Genc, H., E. Morita, N.D. Perrier, D. Miura, P. Ituarte, Q.Y. Duh, O.H. Clark. "Differing Histologic Findings after Bilateral and Focused Parathyroidectomy." Journal of the American College of Surgery 196, no.4 (2003): 535-40.
Goldstein, R.E., D. Billheimer, W.H. Martin, K. Richards. "Sestamibi Scanning and Minimally Invasive Radioguided Parathyroidectomy without Intraoperative Parathyroid Hormone Measurement." Annals of Surgery 237, no.5 (2003): 722-31.
Miccoli, P., P. Berti, G. Materazzi, G. Donatini. "Minimally Invasive Video Assisted Parathyroidectomy (MIVAP)." European Journal of Surgical Oncology 29, no.2 (2003): 188-90.
organizations
American College of Surgeons. 633 North St. Clair Street, Chicago, IL 60611-32311. (312) 202-5000, fax: (312) 202-5001. http://www.facs.org , E-mail: http://postmaster@ facs.org.
American Medical Association. 515 N. State Street, Chicago, IL 60610. (312) 464-5000. http://www.ama-assn.org .
American Academy of Otolaryngology-Head and Neck Surgery. One Prince St., Alexandria, VA 22314-3357. (703) 836-4444. http://www.entnet.org/index2.cfm .
American Osteopathic College of Otolaryngology-Head and Neck Surgery. 405 W. Grand Avenue, Dayton, OH 45405. (937) 222-8820 or (800) 455-9404, fax (937) 222-8840. Email: http://info@aocoohns.org.
Association of Thyroid Surgeons. 717 Buena Vista St., Ventura, CA 93001. Fax: (509) 479-8678. http://info@thyroidsurgery.org.
other
Columbia University Medical Center. [cited May 5, 2003] http://cpmcnet.columbia.edu/dept/thyroid/parasurgHP.html .
Mayo Clinic. [cited May 5, 2003] http://www.mayoclinic.org/checkup/02mar-parathyroid.html .
Ohio State University. [cited May 5, 2003] http://www.acs.ohio-state.edu/units/osuhosp/patedu/Materials/PDFDocs/surgery/thyroid.pdf .
University of California-San Diego. [cited May 5, 2003] http://www-surgery.ucsd.edu/ent/PatientInfo/th_parathyroid.html .
University of Wisconsin. [cited May 5, 2003] http://www.surgery.wisc.edu/general/patients/endocrine.shtml .
L. Fleming Fallon, Jr., M.D., Dr.PH.
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Parathyroidectomy is an operation performed most commonly by a general surgeon, or occasionally by an otolaryngologist, in the operating room of a hospital.
QUESTIONS TO ASK THE DOCTOR
- What type of physician performs the surgery?
- Is the surgeon board certified in head and neck surgery?
- How many parathyroidectomy procedures has the surgeon performed?
- What is the surgeon's complication rate?
- Is there an alternative to surgery?
- What is the risk of complication?
- How will the body's function change after the surgery?