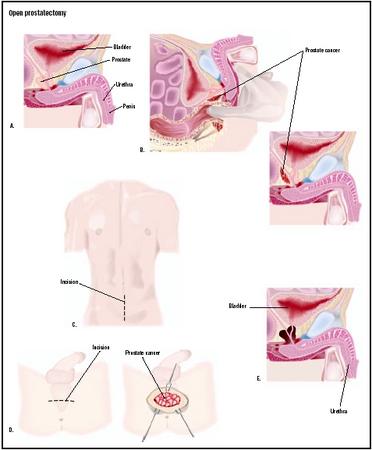
Open prostatectomy
Definition
Open prostatectomy is a procedure for removal of an enlarged prostate gland.
Purpose
The primary indication for open prostatectomy is benign prostatic hyperplasia (BPH), a condition whereby benign or noncancerous nodules grow in the prostate gland. The prostate gland is composed of smooth muscle cells, glandular cells, and cells that give the gland structure (stromal cells). A dense fibrous capsule surrounds the prostate gland. The glandular cells produce a milky fluid that mixes with seminal fluid and sperm to make semen. The prostate gland also produces a hormone (dihydrotestosterone) that has a major impact on the gland's development.
Description
The prostate gland undergoes several changes as a man ages. The pea size gland at birth grows only slightly during puberty, and reaches its normal adult shape and size (similar to a walnut) when a male is in his early twenties. The prostate gland remains stable until the mid-forties. At that time—in most men—the number of cells begins to multiply (cell multiplication), and the gland starts to enlarge. The enlargement—called hyperplasia—is due to an increase in the number of cells. Cell proliferation in the prostates of older men can cause symptoms (referred to as lower urinary tract symptoms, LUTS), which often include:
- straining when urinating
- hesitation before urine flow starts
- dribbling at the end of urination or leakage afterward
- weak or intermittent urinary strain
- painful urination
Other symptoms (called storage symptoms) sometime appear, and may include:
- urgent need to urinate
- bladder pain when urinating
- increased frequency of urination, especially at night
- bladder irritation during urination
The cause of BPH is not fully understood. Currently, it is thought to be caused by a hormone that the prostate gland synthesizes, called dihydrotestosterone (DHT). This hormone is synthesized from testosterone by a prostatic enzyme called 5-alpha reductase.
Surgery is generally indicated for persons with moderate to severe symptoms, particularly if urinary retention is intractable or if the enlarged prostate (BPH) is related to recurrent urinary tract infections, blood in the urine, bladder stones, or kidney problems.
Open prostatectomy is the treatment of choice for approximately 2–3% of BPH patients who have a very large prostate, a damaged bladder, or another serious related problem. Open prostatectomy is used when the prostate is so large (2.8–3.5 oz [80–100 g]) that transurethral resection of the prostate (TURP, a less strenuous surgical procedure to remove a smaller prostate) cannot be performed. Additionally, open prostatectomy is indicated for males with:
- recurrent or persistent urinary tract infections
- acute urinary distention
- bladder outlet obstructions
- recurrent gross hematuria (blood in urine) of prostate origin
- pathological changes in the bladder, ureters, or kidneys due to prostate obstruction
Contraindications to open prostatectomy include previous prostatectomy, prostate cancer, a small fibrous prostate gland, and previous pelvic surgery that may obstruct access to the prostate gland.
Demographics
The cause of BPH is not entirely known; however, the incidence increases with advancing age. Before 40 years of age, approximately 10% of males have BPH. A small amount of hyperplasia is present in 80% of males over 40 years old. Approximately 8–31% of males experience moderate to severe lower urinary tract symptoms (LUTS) in their fifties. By age 80, about 80% of men have LUTS. A risk factor is the presence of normally functioning testicles; research indicates that castration can minimize prostatic enlargement. It appears that the glandular tissues that multiply abnormally use male hormones produced in the testicles differently than the normal tissues do.
Approximately 5.5 million American males have BPH. It is more prevalent in the United States and Europe, and less common among Asians. BPH is more common in men who are married rather than single, and there is a strong genetic correlation. A man's chance for developing BPH is greater if three of more family members have the condition.
Description
Open prostatectomy can be performed by either the retropubic or suprapubic approach. The preferred anesthesia for open prostatectomy is a spinal or epidural nerve block. Regional anesthesia can help reduce blood loss during surgery, and lowers the risk of complications such as pulmonary embolus and postoperative deep vein thrombosis. General anesthesia may be used if the patient has an anatomic or medical contraindication for regional anesthesia.
Retropubic prostatectomy
The retropubic prostatectomy is accomplished through a direct incision of the anterior (front) prostatic capsule. The overgrowth of glandular cells (hyperplastic prostatic adenoma) is removed. These are the cells forming a mass in the prostate because of their abnormal multiplication.
A cystoscopy is performed prior to the open prostatectomy. The patient lies on his back on the operating table, and is prepared and draped for this procedure. Following the cystoscopy, the patient is changed to a Trendelenberg (feet higher than head) position. The surgical area is shaved, draped, and prepared. A catheter is placed in the urethra to drain urine. An incision is made from the umbilicus to the pubic area. The abdominal muscle (rectus abdominis) is separated, and a retractor is placed at the incision site to widen the surgical field. Further maneuvering is essential to clearly locate the veins (dorsal vein complex) and the bladder neck. Visualization of the bladder neck exposes the patient's main arterial blood supply to the prostate gland. Once the structures have been identified and the blood supply controlled, an incision is made deep into the level of the tumor. Scissors are used to dissect the prostatic tissue (prostatic capsule) from the underlying tissue of the prostatic tumor. The wound is closed after complete removal of the prostate tumor and hemostasis (stoppage of bleeding) occurs.
The advantages of the retropubic prostatectomy include:
- Direct visualization of the prostatic tumor.
- Accurate incisions in the urethra, which will minimize the complication of urinary continence.
- Excellent anatomic exposure and visualization of the prostate.
- Clear visualization to control bleeding after tumor removal.
- Little or no surgical trauma to the urinary bladder.
Suprapubic prostatectomy
Suprapubic prostatectomy (also called transvesical prostatectomy) is a procedure to remove the prostatic overgrowth via a different surgical route. The suprapubic approach utilizes an incision of the lower anterior (front) bladder wall. The primary advantage over the retropubic approach is that the suprapubic route allows for direct visualization of the bladder neck and bladder mucosa. Because of this, the procedure is ideally suited for persons who have bladder complications, as well as obese men. The major disadvantage is that visualization of the top part of the tumor is reduced. Additionally, with the subrapubic approach, hemostasis (stoppage of bleeding during surgery) may be more difficult due to poor visualization after removal of the tumor.
Using a scalpel, a lower midline incision is made from the umbilicus to the pubic area. A cystotomy (incision into the bladder) is made, and the bladder inspected. Using electrocautery (a special tool that produces heat at the tip, useful for hemostasis or tissue excision) and scissors, dissection proceeds until the prostatic tumor is identified and removed. After maintaining hemostasis and arterial blood supply to the prostate, the incisions to the bladder and abdominal wall are closed.
Diagnosis/Preparation
The presence of symptoms is indicative of the disease. Age also has an associated risk for an enlarged prostate, and can help establish diagnostic criteria.
Men must have a special blood test called the prostate specific antigen (PSA) and routine digital rectal examination (DRE) before surgery. If the PSA levels and DRE are suspiciously indicative of prostate cancer, a transrectal ultrasound guided needle biopsy of the prostate must be performed before open prostatectomy, to detect the presence of prostate cancer (carcinoma).
Additionally, preoperative patients should have lower urinary tract studies, including urinary flow rate and post void residual urine in the bladder. Because most patients are age 60 or older, preoperative evaluation should also include a detailed history and physical examination ; standard blood tests; chest x ray; and electrocardiogram (EKG) to detect any possible preexisting conditions.
Aftercare
Open prostatectomy is a major surgical operation requiring an inpatient hospital stay of four to seven days. Blood transfusions are generally not required due to improvements in surgical technique. Immediately after the operation, the surgeon must closely monitor urinary output and fluid status. On the first day after surgery, most patients are given a clear liquid diet and asked to sit up four times. Morphine sulfate, given via a patient controlled analgesic pump (IV), is used to control pain.
On the second postoperative day, the urethral catheter is removed if the urine does not contain blood. Oral pain medications are begun if the patient can tolerate a regular diet.
On the third postoperative day, the pelvic drain is removed if drainage is less than 75ml/24 hr. The patient should gradually increase activity. Follow-up with the surgeon is necessary following discharge from the hospital . Full activity is expected to resume within four to six weeks after surgery.
Risks
Improvements in surgical technique have lowered blood loss to a minimal level. For several weeks after open prostatectomy, patients may have urgency and urge incontinence. The severity of bladder problems depends on the patient's preoperative bladder status. Erectile dysfunction occurs in 3–5% of patients undergoing this procedure. Retrograde (backward flow) ejaculation occurs in approximately 50–80% of patients after open prostatectomy. The most common non-urologic risks include pulmonary embolism, myocardial infarction (heart attack), deep vein thrombosis, and cerebrovascular accident (stroke). The incidence of any one of these potentially adverse effects is less than 1%.
Normal results
Normally, patients will not have the adverse effects of bleeding. Hematuria (blood in the urine) is typically resolved within two days after surgery. The patient should begin a regular diet and moderate increases in activity soon after surgery. His pre-surgical activity level should be restored within four to six weeks after surgery.
Morbidity and mortality rates
The overall rate of morbidity and mortality is extremely low. The overall mortality (death) rate for open prostatectomy is approximately zero.
Alternatives
For smaller prostates, treatment using medication may help to control abnormal prostatic growth. When the prostate gland is large (75 grams and bigger), surgery is indicated.
Resources
books
Walsh, P. Campbell's Urology. 8th Ed. St. Louis: Elsevier Science, 2002.
periodicals
Dull, P., R. Reagan, R. Bahnson, "Practical Therapeutics: Managing Benign Prostatic Hyperplasia." American Family Physician 66 (July 1, 2002).
Miles, B., et al."Open Prostatectomy." eMedicine.com [cited July 7, 2003]. http://www.emedicine.com/med/topic3041.htm .
Laith Farid Gulli, M.D., M.S.
Alfredo Mori, M.B.B.S.
Abraham F. Ettaher, M.D.
Bilal Nasser, M.D.,M.S.
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
The procedure is performed by a urological surgeon who typically completes one year of general surgery training, and four to five years of urology training. The procedure is usually performed in a large hospital.
QUESTIONS TO ASK THE DOCTOR
- Why is an open prostatectomy recommended?
- What form of open prostatectomy—retropubic or suprapubic—will be used?
- What forms of anesthesia and pain relief will be given?
- Where will the incision be located?
- What are the risks of the procedure?
- Is the surgeon a board certified urologist?
- Is there an alternative to open prostatectomy?
- What are the chances of after effects, including erectile problems?
thanks
MY HUSBAND HAD OPEN RETROPUBIC PROSTATECTOMY 6 WEEKS ADO, BUT HE STILL HAVE PAIN ON HIS EGGS.
IS IT NORMAL AND HOW LONG IT WILL BE?
THANK YOU
AD
My father had the surgery one week a go and he's still bleeding, is this normal? the Doctors are saying its normal up to 10 days but some of the articles I been reading the bleeding suppose to stop after 2 days, any advice, pls help.thanks
Please advise as what should I do now.
Thank you,
Joe Cefalu
Subhi Sadeek