Vital signs
Definition
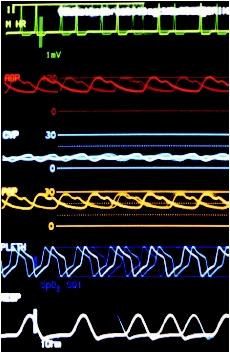
Vital signs, or signs of life, include the following objective measures for a person: temperature, respiratory rate, heart beat (pulse), and blood pressure. When these values are not zero, they indicate that a person is alive. All of these vital signs can be observed, measured, and monitored. This will enable the assessment of the level at which an individual is functioning. Normal ranges of measurements of vital signs change with age and medical condition.
Purpose
The purpose of recording vital signs is to establish a baseline on admission to a hospital, clinic, professional office, or other encounter with a health care provider. Vital signs may be recorded by a nurse, physician, physician's assistant, or other health care professional. The health care professional has the responsibility of interpreting data and identifying any abnormalities from a person's normal state, and of establishing if current treatment or medications are having the desired effect.
Abnormalities of the heart are diagnosed by analyzing the heartbeat (or pulse) and blood pressure. The rate, rhythm and regularity of the beat are assessed, as well as the strength and tension of the beat, against the arterial wall.
Vital signs are usually recorded from once hourly to four times hourly, as required by a person's condition.
The vital signs are recorded and compared with normal ranges for a person's age and medical condition. Based on these results, a decision is made regarding further actions to be taken.
All persons should be made comfortable and reassured that recording vital signs is normal part of health checks, and that it is necessary to ensure that the state of their health is being monitored correctly. Any abnormalities in vital signs should be reported to the health care professional in charge of care.
Description
Temperature
Temperature is recorded to check for fever (pyrexia or a febrile condition), or to monitor the degree of hypothermia.
Manufacturer guidelines should be followed when recording a temperature with an electronic thermometer . The result displayed on the liquid crystal display (LCD) screen should be read, then recorded in a person's medical record. Electronic temperature monitors do not have to be cleaned after use. They have protective guards that are discarded after each use. This practice ensures that infections are not spread.
An alcohol or mercury thermometer can be used to monitor a temperature by three methods:
- Axillary, under the armpit. This method provides the least accurate results.
- Orally, under the tongue. This method is never used with infants or very young children because they may accidentally bite or break the thermometer. They also have difficulty holding oral thermometers under their tongues long enough for their temperatures to be accurately measured.
- Rectally, inserted into the rectum. This method provides the most accurate recording of recording the temperature. It is most often used for infants. A recent study reported that rectal thermometers were more accurate than ear thermometers in detecting high fevers. With the ability to detect low-grade fevers, rectal thermometers can be useful in discovering serious illnesses, such as meningitis or pneumonia. The tip of a rectal thermometer is usually blue, which distinguishes it from the silver tip of an oral, or axillary thermometer.
To record the temperature using an alcohol or mercury thermometer, one should shake down the thermometer by holding it firmly at the clear end and flicking it quickly a few times, with the silver end pointing downward. The health care provider who is taking the temperature should confirm that the alcohol or mercury is below a normal body temperature.
To record an axillary temperature, the silver tip of the thermometer should be placed under the right armpit. The arm clamps the thermometer into place, against the chest. The thermometer should stay in place for three to four minutes. After the appropriate time has elapsed, the thermometer should be removed and held at eye level. During this waiting period, the body temperature will be measured The alcohol or mercury will have risen to a mark that indicates the temperature of a person.
To record an oral temperature, the axillary procedure should be followed, except that the silver tip of the thermometer should be placed beneath the tongue for three to four minutes, then read as described previously.
In both cases, the thermometer should be wiped clean with an antiseptic and stored in an appropriate container to prevent breakage.
To record a rectal temperature, a rectal thermometer should be shaken down, as described previously. A small amount of water-based lubricant should be placed on the colored tip of the thermometer. Infants must be placed on their stomachs and held securely in place. The tip of the thermometer is inserted into the rectum no more than 0.5 in (1.3 cm) and held there for two to three minutes. The thermometer is removed, read as before, and wiped with an antibacterial wipe. It is then stored in an appropriate container to prevent breakage, because ingestion of mercury can be fatal.
Respiratory rate
An examiner's fingers should be placed on the person's wrist, while the number of breaths or respirations in one minute is recorded. Every effort should be made to prevent people from becoming aware that their breathing is being checked. Respiration results should be noted in the medical chart.
Heart beat (pulse)
The pulse can be recorded anywhere that a surface artery runs over a bone. The radial artery in the wrist is the point most commonly used to measure a pulse. To measure a pulse, one should place the index, middle, and ring fingers over the radial artery. It is located above the wrist, on the anterior or front surface of the thumb side of the arm. Gentle pressure should be applied, taking care to avoid obstructing blood flow. The rate, rhythm, strength, and tension of the pulse should be noted. If there are no abnormalities detected, the pulsations can be counted for half a minute, and the result doubled. However, any irregularities discerned indicate that the pulse should be recorded for one minute. This will eliminate the possibility of error. Pulse results should be noted in the health chart.
Blood pressure
To record blood pressure, a person should be seated with one arm bent slightly, and the arm bare or with the sleeve loosely rolled up. With an aneroid or automatic unit, the cuff is placed level with the heart and wrapped around the upper arm, one inch above the elbow. Following the manufacturer's guidelines, the cuff is inflated and then deflated while an attendant records the reading.
If the blood pressure is monitored manually, a cuff is placed level with the heart and wrapped firmly but not tightly around the arm one inch above the elbow over the brachial artery. Wrinkles in the cuff should be smoothed out. Positioning a stethoscope over the brachial artery in front of the elbow with one hand and listening through the earpieces, the cuff is inflated well above normal levels (to about 200 mmHg), or until no sound is heard. Alternatively, the cuff should be inflated 10 mm Hg above the last sound heard. The valve in the pump is slowly opened. Air is allowed to escape no faster than 5 mmHg per second to deflate the pressure in the cuff to the point where a clicking sound is heard over the brachial artery. The reading of the gauge at this point is recorded as the systolic pressure.
The sounds continue as the pressure in the cuff is released and the flow of blood through the artery is no longer blocked. At this point, the noises are no longer heard. The reading of the gauge at this point is noted as the diastolic pressure. "Lub-dub" is the sound produced by the normal heart as it beats. Every time this sound is detected, it means that the heart is contracting once. The noises are created when the heart valves click to close. When one hears "lub," the atrioventricular valves are closing. The "dub" sound is produced by the pulmonic and aortic valves.
With children, the clicking noise does not disappear but changes to a soft muffled sound. Because sounds continue to be heard as the cuff deflates to zero, the reading of the gauge at the point where the sounds change is recorded as the diastolic pressure.
Blood pressure readings are recorded with the systolic pressure first, then the diastolic pressure (e.g., 120/70).
Blood pressure should be measured using a cuff that is correctly sized for the person being evaluated. Cuffs that are too small are likely to yield readings that can be 10 to 50 millimeters (mm) Hg too high. Hypertension (high blood pressure) may be incorrectly diagnosed.
Preparation
As there may be no recorded knowledge of a person's previous vital signs for comparison, it is important that a health care professional be aware that there is a wide range of normal values that can apply to persons of different ages. The health care professional should obtain as detailed a medical history from the person as soon as possible. Any known medical or surgical history, prior measurements of vital signs, and details of current medications should be recorded, as well. Physical exertion prior to measurement of vital signs, such as climbing stairs, may affect the measurements. This should be avoided immediately before the measurement of one's blood pressure. Tobacco, caffeinated drinks, and alcohol should be avoided for 30 minutes prior to recording.
A person should be sitting down or lying comfortably to ensure that the readings are taken in a similar position each time. There should be little excitement, which can affect the results. The equipment required include a watch with a second hand, an electronic or other form of thermometer, an electronic or manual sphygmomanometer with an appropriate sized cuff, and a stethoscope.
Normal results
A normal body temperature taken orally is 98.6°F (37°C), with a range of 97.8–99.1°F (36.5–37.2°C). A fever is a temperature of 101°F (38.3°C) or higher in an infant younger than three months or above 102°F (38.9°C) for older children and adults. Hypothermia is recognized as a temperature below 96°F (35.5°C).
Respirations are quiet, slow, and shallow when the adult is asleep, and rapid, deeper, and noisier during and after activity.
Average respiration rates at rest are:
- infants, 34–40 per minute
- children five years of age, 25 per minute
- older children and adults, 16–20 per minute
Tachypnea is rapid respiration above 20 per minute.
The strength of a heart beat is raised during conditions such as fever and lowered by conditions such as shock or elevated intracranial pressure. The average heart rate for older children (aged 12 and older) and adults is approximately 72 beats per minute (bpm). Tachycardia is a pulse rate over 100 bpm, while bradycardia is a pulse rate of under 60 bpm.
Blood pressure is recorded for older children and adults. A normal adult blood pressure reading is 120/80.
See also Physical examination .
Resources
books
Bickley, L. S., P. G., Szilagyi. J. G. Stackhouse. Bates' Guide to Physical Examination & History Taking, 8th edition. Philadelphia: Lippincott Williams & Wilkins, 2002.
Chan, P. D., and P. J. Winkle. History and Physical Examination in Medicine, 10th ed. New York: Current Clinical Strategies, 2002.
Seidel, Henry M. Mosby's Physical Examination Handbook, 4th ed. St. Louis: Mosby-Year Book, 2003.
Swartz, Mark A., and William Schmitt. Textbook of Physical Diagnosis: History and Examination, 4th edition. Philadelphia: Saunders, 2001.
periodicals
Ahmed A. M. "Deficiences of Physical Examination Among Medical Students." Saudi Medical Journal 24, no. 1 (2003): 108-111.
organizations
American Academy of Family Physicians, 11400 Tomahawk Creek Parkway, Leawood, KS 66211-2672. (913) 906-6000. E-mail: http://fp@aafp.org. http://www.aafp.org .
American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, IL 60007-1098. 847) 434-4000. Fax: (847) 434-8000. E-mail: http://kidsdoc@aap.org. http://www.aap.org/default.htm .
American College of Physicians. 190 N. Independence Mall West, Philadelphia, PA 19106-1572. (800) 523-1546, x2600 or (215) 351-2600. http://www.acponline.org .
other
Karolinska Institute. [cited March 1, 2003] http://isp.his.ki.se/text/physical.htm .
Loyola University Chicago Stritch School of Medicine. [cited March 1, 2003] http://www.meddean.luc.edu/lumen/MedEd/MEDICINE/PULMONAR/PD/Pdmenu.htm .
National Library of Medicine. [cited March 1, 2003] http://www.nlm.nih.gov/medlineplus/ency/article/002274.htm .
Review of Systems School of Medical Transcription. [cited March 1, 2003] http://www.mtmonthly.com/studentcorner/cpe.htm .
L. Fleming Fallon, Jr., M.D., DrPH
Thanks..thanks and more power.....
pray for my success...
THANKS SO MUCH
What time is it necessary to take vital signs??