Small bowel resection
Definition
A small bowel resection is the surgical removal of one or more segments of the small intestine.
Purpose
The small intestine is the part of the digestive system that absorbs much of the liquid and nutrients from food. It consists of three segments: the duodenum, jejunum, and ileum; and is followed by the large intestine (colon). A small bowel resection may be performed to treat the following conditions:
- Crohn's disease. This condition is characterized by a chronic inflammatory condition that affects the digestive tract. If other treatment does not effectively control symptoms, the physician may recommend surgery to close fistulas or remove part of the intestine where the inflammation is worst.
- Cancer. Cancer of the small intestine is a rare cancer in which malignant cells are found in the tissues of the small intestine. Adenocarcinoma, lymphoma, sarcoma, and carcinoid tumors account for the majority of small intestine cancers. Surgery to remove the cancer is the most common treatment. When the tumor is large, removal of the small intestine segment containing the cancer is usually indicated.
- Ulcers. Ulcers are crater-like lesions on the mucous membrane of the small bowel caused by an inflammatory, infectious, or malignant condition that often requires surgery and in some cases, bowel resection.
-
Intestinal obstruction. This condition involves a partial or complete
blockage of the bowel that results in the failure of the intestinal
contents to pass through. Intestinal obstruction is usually treated by
decompressing the intestine with suction, using a nasogastric
tube inserted into the stomach or intestine. In cases where decompression does not relieve the symptoms, or if tissue death is suspected, bowel resection may be considered.
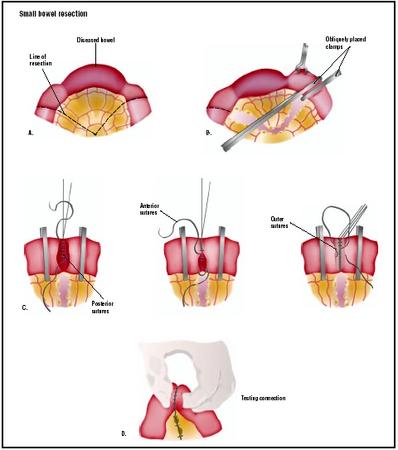 To remove a diseased portion of the small intestine, an incision is made into the abdomen, and the area to be treated is pulled out (A). Clamps are placed around the area to be removed and the section is cut (B). Three layers of sutures repair the remaining bowel (C). (Illustration by GGS Inc.)
To remove a diseased portion of the small intestine, an incision is made into the abdomen, and the area to be treated is pulled out (A). Clamps are placed around the area to be removed and the section is cut (B). Three layers of sutures repair the remaining bowel (C). (Illustration by GGS Inc.) - Injuries. Accidents may result in bowel injuries that require resection.
- Precancerous polyps. A polyp is a growth that projects from the lining of the intestine. Polyps are usually benign and produce no symptoms, but they may cause rectal bleeding and develop into malignancies over time. When polyps have a high chance of becoming cancerous, bowel resection is usually indicated.
Demographics
According to the National Cancer Institute, adenocarcinoma, lymphoma, sarcoma, and carcinoid tumors account for the majority of small intestine cancers which, as a whole, account for only 1–2% of all gastrointestinal cancers diagnosed in the United States.
Crohn's disease occurs worldwide with a prevalence of 10–100 cases per 100,000 people. The disorder occurs most frequently among people of European origin; is three to eight times more common among Jews than among non-Jews; and is more common among whites than nonwhites. Although the disorder can start at any age, it is most often diagnosed between 15 and 30 years of age. Some 20–30% of patients with Crohn's disease have a family history of inflammatory bowel disease.
The occurrence of polyps increases with age; the risk of cancer developing in an unremoved polyp is 2.5% at five years, 8% at 10 years, and 24% at 20 years after the diagnosis. The risk of developing bowel cancer after removal of polyps is 2.3%, compared to 8.0% for patients who do not have them removed.
Description
The resection procedure can be performed using an open surgical approach or laparoscopically. There are three types of surgical small bowel resection procedures:
- Duodenectomy. Excision of all or part of the duodenum.
- Ileectomy. Excision of all or part of the ileum.
- Jejunectomy. Excision of all or a part of the jejunum.
Open resection
Following adequate bowel preparation, the patient is placed under general anesthesia and positioned for the operation. The surgeon starts the procedure by making a midline incision in the abdomen. The diseased part of the small intestine (ileum or duodenum or jejunum) is removed. The two healthy ends are either stapled or sewn back together, and the incision is closed. If it is necessary to spare the intestine from its normal digestive work while it heals, a temporary opening (stoma) of the intestine into the abdomen ( ileostomy , duodenostomy, or jejunostomy) is made. The ostomy is later closed and repaired.
Laparoscopic bowel resection
Laparoscopic small bowel resection features insertion of a thin telescope-like instrument called a laparoscope through a small incision made at the umbilicus (belly button). The laparoscope is connected to a small video camera unit that shows the operative site on video monitors located in the operating room . The abdomen is inflated with carbon dioxide gas to allow the surgeon a clear view of the operative area. Four to five additional small incisions are made in the abdomen for insertion of specialized surgical instruments that the surgeon uses to perform the surgery. The small bowel is clamped above and below the diseased section and this section is removed. The small bowel ends are reattached using staples or sutures. Following the procedure, the small incisions are closed with sutures or surgical tape.
Diagnosis/Preparation
As with any surgery, the patient is required to sign a consent form. Details of the procedure are discussed with the patient, including goals, technique, and risks. Blood and urine tests, along with various imaging tests and an electrocardiogram (EKG), may be ordered as required. To prepare for the procedure, the patient is asked to completely clean the bowel and is placed on a low residue diet for several days prior to surgery. A liquid diet may be ordered for at least the day before surgery, with nothing taken by mouth after midnight. Preoperative bowel preparation involving mechanical cleansing and administration of antibiotics before surgery is the standard practice. This involves the prescription of oral antibiotics (neomycin, erythromycin, or kanamycin sulfate) to decrease bacteria in the intestine and help prevent postoperative infection. A nasogastric tube is inserted through the nose into the stomach on the day of surgery or during surgery. This removes the gastric secretions and prevents nausea and vomiting. A urinary catheter (thin tube inserted into the bladder) may also be inserted to keep the bladder empty during surgery, giving more space in the surgical field and decreasing chances of accidental injury.
Aftercare
Once the surgery is completed, the patient is taken to a postoperative or recovery unit where a nurse monitors recovery and ensures that bandages are kept clean and dry. Mild pain at the incision site is commonly experienced and the treating physician usually prescribes pain medication. Postoperative care also involves monitoring of blood pressure, pulse, respiration, and temperature. Breathing tends to be shallow because of the effect of anesthesia and the patient's reluctance to breathe deeply and experience pain that is caused by the abdominal incision. The patient is given instruction on the way to support the operative site during deep breathing and coughing. Fluid intake and output is measured, and the operative site is observed for color and amount of wound drainage. The nasogastric tube remains in place, attached to low intermittent suction until bowel activity resumes. Fluids and electrolytes are infused intravenously until the patient's diet can gradually be resumed, beginning with liquids and progressing to a regular diet as tolerated. The patient is generally out of bed approximately eight to 24 hours after surgery. Patients are usually scheduled for a follow-up examination within two weeks after surgery. During the first few days after surgery, physical activity is restricted.
Risks
Risks include all the risks associated with general anesthesia, namely, adverse reactions to medications and breathing problems. They also include the risks associated with any surgery, such as bleeding or infection. Additional risks associated specifically with bowel resection include:
- bulging through the incision (incisional hernia)
- narrowing (stricture) of the opening (stoma)
- blockage (obstruction) of the intestine from scar tissue.
Normal results
Complete healing is expected without complications after bowel resection, but the period of time required for recovery from the surgery varies depending on the condition requiring the procedure, the patient's overall health status prior to surgery, and the length of bowel removed.
Morbidity and mortality rates
According to the National Cancer Institute, the predominant treatment for small intestine cancers is surgery when bowel resection is possible, and cure depends on the ability to completely remove the cancer. The overall five-year survival rate for resectable adenocarcinoma is 20%. The five-year survival rate for resectable leiomyosarcoma, the most common primary sarcoma of the small intestine, is approximately 50%.
Crohn's disease is a chronic incurable disease characterized by periods of progression and remission with 99% of patients suffering at least one relapse. Physicians are presently unable to predict the extent and severity of the disease over time; thus, while morbidity is very high for Crohn's disease, mortality is essentially zero.
Alternatives
Alternatives to bowel resection depend on the specific medical condition being treated. For most conditions where bowel resection is advised, the only alternative is treatment with drugs.
Resources
books
Michelassi, F. and J. W. Milsom, eds. Operative Strategies in Inflammatory Bowel Disease. New York: Springer Verlag, 1999.
Peppercorn, Mark, ed. Therapy of Inflammatory Bowel Disease: New Medical and Surgical Approaches. New York: Marcel Dekker, 1989.
Ratnaike, R. N., ed. Small Bowel Disorders. London: Edward Arnold, 2000.
Thompson, J. C., and L. Rose. Atlas of Surgery of the Stomach, Duodenum, and Small Bowel. St. Louis: Mosby, 1992.
periodicals
Bines, J. E., R. G. Taylor, F. Justice, et al. "Influence of Diet Complexity on Intestinal Adaptation Following Massive Small Bowel Resection in a Preclinical Model." Journal of Gastroenterology and Hepatology 17 (November 2002): 1170–1179.
Dahly, E. M., M. B. Gillingham, Z. Guo, et al. "Role of Luminal Nutrients and Endogenous GLP-2 in Intestinal Adaptation to Mid-Small Bowel Resection." American Journal of Physiology and Gastrointestinal Liver Physiology 284 (March 2003): G670–G682.
Libsch, K. D., N. J. Zyromski, T. Tanaka, et al. "Role of Extrinsic Innervation in Jejunal Absorptive Adaptation to Subtotal Small Bowel Resection: A Model of Segmental Small Bowel Transplantation." Journal of Gastrointestinal Surgery 6 (March-April 2002): 240–247.
O'Brien, D. P., L. A. Nelson, J. L. Williams, et al. "Selective Inhibition of the Epidermal Growth Factor Receptor Impairs Intestinal Adaptation After Small Bowel Resection." Journal of Surgical Research 105 (June 2002): 25–30.
organizations
American Board of Colorectal Surgeons (ABCRS). 20600 Eureka Rd., Ste. 600, Taylor, MI 48180. (734) 282-9400. http://www.abcrs.org .
American Society of Colorectal Surgeons (ASCRS). 85 West Algonquin, Suite 550, Arlington Heights, IL 60005. (847) 290 9184. http://www.fascrs.org .
United Ostomy Association, Inc. (UOA). 19772 MacArthur Blvd., Suite 200, Irvine, CA 92612-2405. (800) 826-0826. http://www.uoa.org .
other
"Bowel Resection; Patient Discharge Instructions." Northwest Memorial Hospital Patient Education Brochure . March 2001 [cited June 25, 2003]. http://www.nmh.org/patient_ed_pdfs/pt_ed_bowel_resection_discharge.pdf. .
"Crohn's Disease." American Society of Colon and Rectal Surgeons Patient Brochure. 1996 [cited June 25, 2003]. http://www.fascrs.org .
Monique Laberge, Ph.D.
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Bowel resection surgery is performed by a colorectal surgeon, who is a physician fully trained in general surgery as evidenced by certification by the American Board of Surgery (ABS). Colorectal surgeons also are certified by the American Society of Colon and Rectal Surgeons (ASCRS), the leading professional society representing more than 1,000 board-certified colon and rectal surgeons and other surgeons dedicated to advancing and promoting the science and practice of the treatment of patients with diseases and disorders affecting the colon, rectum, and anus.
Bowel resection surgery is performed in a hospital setting.
QUESTIONS TO ASK THE DOCTOR
- What do I need to do before surgery?
- What happens on the day of surgery?
- What type of anesthesia will be used?
- What happens during surgery, and how is the surgery performed?
- What happens after the surgery?
- What are the risks associated with a small bowel resection?
- How long will I be in the hospital?
- When can I expect to return to work and/or normal activities?
- Will there be a scar?
Dr. removed 8 in small intestine and part of stomach, and 3 lymph nodes. I'm home now and doing good. I have to really be careful not to eat too much, makes me feel uncomfortable if I eat just a little too much. My concern now is a return of the carcinoid tumor. I should be back to work by Dec 14th. My first time to have surgery, guess I'm doing ok for a 63 year old man.
Delores Reno
Delores, my partner has suffered from Crohns Disease for the past 6 years (but only diagnosed in July 2010)and had a bowel resection (laproscopic illeocecal resection) on 11 Feb 2011. The next day he was good but on the Sunday he was in a lot of pain and by Sunday night had temps of 39/40 degress celcius (FYI we are in Australia). They performed a CT scan on Monday which showed nothing and his temps continued to go up and down all week. They ran blood tests etc everyday as the ones from Monday indicated an infection in his body somewhere. He was also at that point pumped full of antibiotics. His legs also swelled up even though he had those stockings on that they make you wear. He was also extremely bloated. They performed a 2nd CT scan with contrast on Thursday (17 Feb)and they found a leak in his bowel - they could not determine where it was but could see the gas etc leaking into his abdomen. He was prepped for emergency surgery that night and this time it was open surgery. The surgery was complicated as they couldn't actually see a hole or anything where the leak could be. He now has a temporary colostomy bag (which he will have for about 2mths) to give his bowels etc time to heal. I am currently 37wks pregnant and have an 18mth old son so I did not travel with him for him to have the surgery but luckily his parents live near the hospital where the surgery needed to be done so have been able to be there for him and pass on information to me. Anyway as I have not been there I haven't had a chance to speak with the drs but it sounds a lot like perotonitis (inflammation of the gastro system)as what your daughter had. He will be in hospital until atleast Monday where they will assess his state of recovery and cease the morphine injections.
I am so very sorry to hear that your daughter lost her life and I feel so very lucky that the drs have done everything possible to sort him out. He is doing much better already and has not even been out of surgery 24hrs yet.
I eventually had to have a small bowel resection in Sept 2010, as scar tissue had formed at the damaged part of my bowel and it had pretty much closed up. I had open surgery which was extremely successful, and I have felt great ever since. Recovery was difficult (painful), but I made progress each day so I never felt disheartened. Crohn's can of course return at any time, so I count myself lucky every day.
As surgery is not a cure and can, in some people, make things worse, your doctor will be trying to get you into remission through the use of drugs first. Although surgery will probably be inevitable at some stage. I used to think of surgery as 'opening a can of worms', and maybe it is. But for me, it was definitely the right decision and has given me my life back.
Just remember to listen to your body and do what is right for you.
After speaking with him i was put on 2 different kinds of antibiotics and prednisone in addition to my immunosuppressant. The antibiotics along with prescription painkillers appeared to be working. However, a few weeks later the same symptoms returned. I was sweating and pale, my heart was racing due to an infection that was progressing in my body. The gastrointerologist finally recommended i turn to a surgeon for a consultation. Which was a relief to me, as i knew at this point was the only rational course of action. In fact, i had felt this way for a while.
I was scanned once more when i was admitted into the hospital awaiting the resection. They pinpointed the problem, a perforation which had not responded to medications. The next day i was in surgery prep receiving a spinal block and anesthesia.
I woke 2 hours later in the recovery room and spent 3 days in the hospital. Thats right, i was released after 3 days. I had 13 staples closing about 6 inches worth of incision beneath my belly button. I spent a lot of time in the bathroom. Still at times my trips to the restroom are frequent. I feel better than i did just prior to surgery but i know my life will always be a little different than before i went under. Surgery is stressful and scary to undergo. Good luck
good until recently. He has a hernia now from it not healing correctly since he's also on chemotherapy
for liver cancer. He has been experiencing a lot of bloating all of a sudden. We're thinking about
making an appointment with the doctor to see if this is a normal side effect. Has anyone else
experienced this?
Thank you
Dee
Thank you
Dee
i had laparotomy and small bowel resection surgery for crown's disease strictures
i had the surgery on 10/12/2013
i am recovery from the surgery i was in hospital for 7 days i am still in horrific pain
my surgeon said it was worst she's ever seen there was 20 strictures and they 1 meter of small bowel
thanks michael
Thanks anyone for comments in advance
Thank you
Margaret
Worried sister,
Mel
Your suggestions and comments are appreciated.