Bowel resection
Definition
Bowel resection is a surgical procedure in which a diseased part of the large intestine is removed. The procedure is also known as colectomy, colon removal, colon resection, or resection of part of the large intestine.
Purpose
The large bowel, also called the large intestine, is a part of the digestive system. It runs from the small bowel (small intestine) to the rectum, which receives waste material from the small bowel. Its major function is to store waste and to absorb water from waste material. It consists of the following sections, any of which may become diseased:
- Colon. The colon averages some 60 in (150 cm) in length. It is divided into four segments: the ascending colon, transverse colon, descending colon, and sigmoid colon. There are two bends (flexures) in the colon. The hepatic flexure is where the ascending colon joins the transverse colon. The splenic flexure is where the transverse colon merges into the descending colon.
- Cecum. This is the first portion of the large bowel that is joined to the small bowel. The appendix lies at the lowest portion of the cecum.
- Ascending colon. This segment is about 8 in (20 cm) in length, and it extends upwards from the cecum to the hepatic flexure near the liver.
- Transverse colon. This segment is usually more than 18 in (46 cm) in length and extends across the upper abdomen to the splenic flexure.
- Descending colon. This segment is usually less than 12 in (30 cm) long and extends from the splenic flexure downwards to the start of the pelvis.
- Sigmoid colon. An S-shaped segment that measures about 18 in (46 cm); it extends from the descending colon to the rectum.
The wall of the colon is composed of four layers:
- Mucosa. This single layer of cell lining is flat and regenerates itself every three to eight days. Small glands lie beneath the surface.
- Submucosa. The area between the mucosa and circular muscle layer that is separated from the mucosa by a thin layer of muscle, the muscularis mucosa.
- Muscularis propria. The inner circular and outer longitudinal muscle layers.
- Serosa. The outer, single-cell, thick covering of the bowel. It is similar to the peritoneum, the layer of cells that lines the abdomen.
The large intestine is also responsible for bacterial production and absorption of vitamins. Resection of a portion of the large intestine (or of the entire organ) may become necessary when it becomes diseased. The exact
- Cancer. Colon cancer is the second most common type of cancer diagnosed in the United States. Colon and rectum cancers, which are usually referred to as colorectal cancer, grow on the lining of the large intestine. Bowel resection may be indicated to remove the cancer.
- Diverticulitis. This condition is characterized by the inflammation of a diverticulum, especially of diverticula occurring in the colon, which may undergo perforation with abscess formation. The condition may be relieved by resecting the affected bowel section.
- Intestinal obstruction. This condition involves a partial or complete blockage of the bowel that results in the failure of the intestinal contents to pass through. It is usually treated by decompressing the intestine with suction, using a nasogastric tube inserted into the stomach or intestine. In cases where decompression does not relieve the symptoms, or if tissue death is suspected, bowel resection may be considered.
- Ulcerative colitis. This condition is characterized by chronic inflammation of the large intestine and rectum resulting in bloody diarrhea. Surgery may be indicated when medical therapy does not improve the condition. Removal of the colon is curative and also removes the risk of colon cancer. About 25–40% of ulcerative colitis patients must eventually have their colons removed because of massive bleeding, severe illness, rupture of the colon, or risk of cancer.
- Traumatic injuries. Accidents may result in bowel injuries that require resection.
- Pre-cancerous polyps. A colorectal polyp is a growth that projects from the lining of the colon. Polyps of the colon are usually benign and produce no symptoms, but they may cause rectal bleeding and develop into malignancies over time. When polyps have a high chance of becoming cancerous, bowel resection may be indicated.
- Familial adenomatous polyposis (FAP). This is a hereditary condition caused by a faulty gene. Most people discover that they have it at a young age. People with FAP grow many polyps in the bowel. These are mostly benign, but because there are so many, it is really only a question of time before one becomes cancerous. Since people with FAP have a very high risk of developing bowel cancer, bowel resection is thus often indicated.
- Hirschsprung's disease (HD). This condition usually occurs in children. It causes constipation, meaning that bowel movements are difficult. Some children with HD cannot have bowel movements at all; the stool creates a blockage in the intestine. If HD is not treated, stool can fill up the large intestine and cause serious problems such as infection, bursting of the colon, and even death.
Description
Bowel resection can be performed using an open surgical approach (colectomy) or laparoscopically.
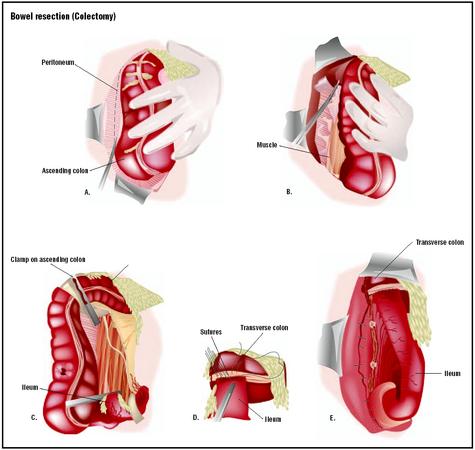
Colectomy
Following adequate bowel preparation, the patient is placed under general anesthesia, which ensures that the patient is deep asleep and pain free during surgery. Because the effects of gravity to displace tissues and organs away from the site of operation are important, patients are carefully positioned, padded, and strapped to the operating table to prevent movement as the patient is tilted to an extreme degree. The surgeon starts the procedure by making a lower midline incision in the abdomen or, alternatively, he may prefer to perform a lateral lower transverse incision instead. He proceeds with the removal of the diseased portion of the large intestine, and then sutures or staples the two healthy ends back together before closing the incision. The amount of bowel removed can vary considerably, depending on the reasons for the operation. When possible, the procedure is performed to maintain the continuity of the bowel so as to preserve normal passage of stool. If the bowel has to be relieved of its normal digestive work while it heals, a temporary opening of the colon onto the skin of abdominal wall, called a colostomy , may be created. In this procedure, the end of the colon is passed through the abdominal wall and the edges are sutured to the skin. A removable bag is attached around the colostomy site so that stool may pass into the bag, which can be emptied several times during the day. Most colostomies are temporary and can be closed with another operation at a later date. However, if a large portion of the intestine is removed, or if the distal end of the colon is too diseased to reconnect to the proximal intestine, the colostomy is permanent.
Laparoscopic bowel resection
The benefits of laparoscopic bowel resection when compared to open colectomies include reduced postoperative pain, shorter hospitalization periods, and a faster return to normal activities. The procedure is also minimally invasive. When performing a laparoscopic procedure, the surgeon makes three to four small incisions in the abdomen or in the umbilicus (belly button). He inserts specialized surgical instruments , including a thin, telescope-like instrument called a laparoscope, in an incision. The abdomen is then filled with gas, usually carbon dioxide, to help the surgeon view the abdominal cavity. A camera is inserted through one of the tubes and displays images on a monitor located near the operating table to guide the surgeon as he works. Once an adequate view of the operative field is obtained, the actual dissection of the colon can start. Following the procedure, the small incisions are closed with sutures or surgical tape.
All colon surgery involves only three maneuvers that may vary in complexity depending on the region of the bowel and the nature of the disease. These three maneuvers are:
- retraction of the colon
- division of the attachments to the colon
- dissection of the mesentery
In a typical procedure, after retracting the colon, the surgeon proceeds to divide the attachments to the liver and the small bowel. Once the mesenteric vessels have been dissected and divided, the colon is divided with special stapling devices that close off the bowel while at the same time cutting between the staple lines. Alternatively, a laparoscopically assisted procedure may be selected, in which a small abdominal wall incision is made at this point to bring the bowel outside of the abdomen, allowing open bowel resection and reconnection using standard instruments. This technique is popular with many surgeons because an incision must be made to remove the bowel specimen from the abdomen, which allows the most time-consuming and risky parts of the procedure (from an infection point of view) to be done outside the body with better control of the colon.
Diagnosis/Preparation
Key elements of the physical examination before surgery focus on a thorough examination of the abdomen, groin, and rectum. Other common diagnostic tools used to evaluate medical conditions that may require bowel resection include imaging tests such as gastrointestinal barium series, angiography , computerized tomography (CT), magnetic resonance imaging (MRI), and endoscopy.
As with any surgery, the patient is required to sign a consent form. Details of the procedure are discussed with the patient, including goals, technique, and risks. Blood and urine tests, along with various imaging tests and an electrocardiogram (EKG), may be ordered. To prepare for the procedure, the patient is asked to completely clean out the bowel. This is a crucial step if the bowel is to be opened safely within the peritoneal cavity, or even manipulated safely through small incisions. To empty and cleanse the bowel, the patient is usually placed on a low-residue diet for several days prior to surgery. A liquid diet may be ordered for at least the day before surgery, with nothing taken by mouth after midnight. A series of enemas and/or oral preparations (GoLytely or Colyte) may be ordered to empty the bowel of stool. Preoperative bowel preparation involving mechanical cleansing and administration of intravenous antibiotics immediately before surgery is the standard practice. The patient may also be given a prescription for oral antibiotics (neomycin, erythromycin, or kanamycin sulfate) the day before surgery to decrease bacteria in the intestine and to help prevent post-operative infection. A nasogastric tube is inserted through the nose into the stomach during surgery and may be left in place for 24–48 hours after surgery. This removes the gastric secretions and prevents nausea and vomiting. A urinary catheter (a thin tube inserted into the bladder) may be inserted to keep the bladder empty during surgery, giving more space in the surgical field and decreasing chances of accidental injury.
Aftercare
Postoperative care for the patient who has undergone a bowel resection, as with those who have had any major surgery, involves monitoring of blood pressure, pulse, respiration, and temperature. Breathing tends to be shallow because of the effect of anesthesia and the patient's reluctance to breathe deeply and experience pain that is caused by the abdominal incision. The patient is instructed how to support the operative site during deep breathing and coughing, and is given pain medication as necessary. Fluid intake and output is measured, and the operative site is observed for color and amount of wound drainage. The nasogastric tube will remain in place, attached to low intermittent suction until bowel activity resumes. Fluids and electrolytes are infused intravenously until the patient's diet can gradually be resumed, beginning with liquids and advancing to a regular diet as tolerated. The patient is generally out of bed approximately eight to 24 hours after surgery. Most patients will stay in the hospital for five to seven days, although laparoscopic surgery can reduce that stay to two to three days. Postoperative weight loss follows almost all bowel resections. Weight and strength are slowly regained over a period of months. Complete recovery from surgery may take two months. Laparoscopic surgery can reduce this time to one to two weeks.
The treating physician should be informed of any of the following problems after surgery:
- increased pain, swelling, redness, drainage, or bleeding in the surgical area
- headache, muscle aches, dizziness, or fever
- increased abdominal pain or swelling, constipation, nausea or vomiting, rectal bleeding, or black, tarry stools
Risks
Potential complications of bowel resection surgery include:
- excessive bleeding
- surgical wound infection
- incisional hernia (an organ projecting through the surrounding muscle wall, it occurs through the surgical scar)
- thrombophlebitis (inflammation and blood clot to veins in the legs)
- narrowing of the opening (stoma)
- pneumonia
- pulmonary embolism (blood clot or air bubble in the lung blood supply)
- reaction to medication
- breathing problems
- obstruction of the intestine from scar tissue
Normal results
Complete healing is expected without complications after bowel resection, but the period of time required for recovery from the surgery varies depending on the initial condition that required the procedure, the patient's overall health status prior to surgery, and the length of bowel removed.
Morbidity and mortality rates
Prognosis for bowel resection depends on the seriousness of the disease. For example, primary treatment for colorectal cancer consists of wide surgical resection of the colon cancer and lymphatic drainage after the bowel is prepared. The choice of operation for rectal cancer depends on the tumor's distance from the anus and gross extent; overall surgical cure is possible in 70% of these patients. In the case of ulcerative colitis patients, the colitis is cured by bowel resection and most people go on to live normal, active lives. As for Hirschsprung's disease patients, approximately 70–85% eventually achieve excellent results after surgery, with normal bowel habits and infrequent constipation.
Alternatives
Alternatives to bowel resection depend on the specific medical condition being treated. For most conditions where bowel resection is advised, the only alternative is medical treatment with drugs. In cases of cancer of the bowel, drug treatment alone will not cure the disease. Occasionally, it is possible to remove a rectal cancer from within the back passage without major surgery, but this only applies to very special cases. As for other conditions such as mild or moderate ulcerative colitis, drug therapy may represent an alternative to surgery; a combination of the drugs sulfonamide, sulfapyridine, and salicylate may help control inflammation. Similarly, most acute cases of diverticulitis are first treated with antibiotics and a liquid diet.
See also Laparoscopy ; Small bowel resection .
Resources
books
Corman, M. L. Colon and Rectal Surgery. Philadelphia: Lippincott Williams & Wilkins, 1998.
Hampton, Beverly, and Ruth Bryant. Ostomies and Continent Diversions. St. Louis: Mosby Inc., 1992.
Michelassi, F., and J. W. Milsom, eds. Operative Strategies in Inflammatory Bowel Disease. New York: Springer Verlag, 1999.
Peppercorn, Mark, ed. Therapy of Inflammatory Bowel Disease: New Medical and Surgical Approaches. New York: Marcel Dekker, 1989.
periodicals
Alves, A., Y. Panis, D. Trancart, J. Regimbeau, M. Pocard, and P. Valleur. "Factors Associated with Clinically Significant Anastomotic Leakage after Large Bowel Resection: Multivariate Analysis of 707 Patients." World Journal of Surgery 26 (April 2002): 499–502.
Miller, J., and A. Proietto. "The Place of Bowel Resection in Initial Debulking Surgery for Advanced Ovarian Cancer." Australian and New Zealand Journal of Obstetrics and Gynaecology 42 (November 2002): 535–537.
Sukhotnik, I., A. S. Gork, M. Chen, R. Drongowski, A. G. Coran, and C. M. Harmon. "Effect of Low Fat Diet on Lipid Absorption and Fatty-acid Transport following Bowel Resection." Pediatric Surgery International 17 (May 2001): 259–264.
Tabet, J., D. Hong, C. W. Kim, J. Wong, R. Goodacre, and M. Anvari. "Laparoscopic versus Open Bowel Resection for Crohn's Disease." Canadian Journal of Gastroenterology 15 (April 2001): 237–242.
Taylor, C., and C. Norton. "Information Booklets for Patients with Major Bowel Resection." British Journal of Nursing 19 (June–July 2000): 785–791.
organizations
American Board of Colorectal Surgeons (ABCRS). 20600 Eureka Rd., Ste. 600, Taylor, MI 48180. (734) 282-9400. http://www.abcrs.org .
The American Society of Colorectal Surgeons (ASCRS). 85 West Algonquin, Suite 550, Arlington Heights, IL 60005. (847) 290 9184. http://www.fascrs.org .
United Ostomy Association, Inc. (UOA). 19772 MacArthur Blvd., Suite 200, Irvine, CA 92612-2405. (800) 826-0826. http://www.uoa.org .
other
"Bowel Resection." Patient & Family Education / NYU Medical Center. http://www.nmh.org/patient_ed_pdfs/pt_ed_bowel_resection_discharge.pdf. .
"Bowel Resection with Colostomy." Health Care Corporation of St. John's. http://www.hccsj.nf.ca/2002/Med_Services/Surgery/Procedures/bowel_resec_col.asp .
"Colorectal Cancer." ASCRS Homepage. http://www.fascrs.org .
Kathleen D. Wright, RN Monique Laberge, PhD
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Bowel resection surgery is performed by a colorectal surgeon, who is a medical doctor fully trained in general surgery and certified by the American Board of Surgery (ABS) as well as by the American Society of Colon and Rectal Surgeons (ASCRS). The surgeon must pass the American Board of Surgery Certifying Examination and complete an approved colorectal training program. The surgeon is then eligible to take the qualifying examination in colorectal surgery after completing training. There is also a certifying examination that is taken after passing the qualifying examination. The surgeon is required to re-certify in surgery in order to re-certify in colon and rectal surgery (every 10 years).
Bowel resection surgery is a major operation performed in a hospital setting. The cost of the surgery varies significantly between surgeons, medical facilities, and regions of the country. Patients who are sicker or need more extensive surgery will require more intensive and expensive treatment.
QUESTIONS TO ASK THE DOCTOR
- What alternatives to bowel resection might be indicated in my case?
- Am I a candidate for bowel resection?
- How many patients with my specific condition have you treated?
- How long will it take to recover from surgery?
- What do I need to do before surgery?
- What happens on the day of surgery?
- What type of anesthesia will be used?
- What happens during surgery, and how is the surgery performed?
Good site though and you have answered some of my fears and questions.
I am 58 yrs and fit.
Regareds,
Afrah
SEVERE DIVERTICULOS AND CONSTANT PAIN, I AM HAVING THE SURGERY ON THE 2ND OF JANUARY.HE TOLD ME NOT TO WALK UP ANY STAIRS, BUT TO GET TO MY BEDROOM I HAVE TO.I AM NOT EATING ANY BEEF AT ALL
ONLY CHICKEN, FISH AND TURKEY AND PEABUTTER SANDWICHES. I AM
TRYING TO RID MY BODY OF ANYTHING THAT CAN CAUSE INFECTION.
I HAVE TO STAY IN FOR 6 DAYS WITH THE FIRST THREE DAYS NOTHING TO EAT OR DRINK.WILL THEY ALSO GIVE ME A MORPHINE PUMP OR HOW DO I
HANDLE THE PAIN, HE IS JUST GOING TO DO IT ENDOSCOPY AND PUT
A SMALL INCISION IN MY LEFT SIDE.DOES HE BURN THE INTESTINE TOGETHER,BECAUSE I DON'T WANT THE STAPELS. IT WOULD MAKE NO
SENSE.HE SAID AFTER 3 DAYS THAT HE WOULD GIVE ME ICE CHIPS.
WILL I GET FED THROUGH A TUBE OR WHAT?
So far, I still run to the bathroom about 1 to 2 times a week. From what I understand, the urge is compared to child birth labor (urge). I suspect this stems from not having the A-colon. On average, I have bowel movements 3 times a day. Somedays it is only 1, somedays it is 6 to 7 times a day. Hard to say why; have not found a pattern yet. Except for bready or doughy food products, my diet has changed little. Although, I have made it common to not eat as much fast-food or spicy foods.
Notwithstanding the extra gas and loud processing of the food and evidence of surgery, I feel pretty normal. But I am fairly certain I will never have constipation or very solid stools. And I better plan long trips or longer times away from a bathroom/restroom.
If anyone has more comments insight or just questions and wants an exchange of thoughts, email me at sdflipper@yahoo.com. Use some website reference so I know it probably wont be spam. I read my email about once a week.
Thanks for the help :)
Can anyone tell me if this is how things are done considering my history or are they just letting me know the worst case scenario.
Regards
Mark
Can you tell me what is going on with my body. How did this material get loose (about 10 inches came out and still some in there). Is there any danger of infection. what is it stuck on?
I called the surgon's office but can't get into see him for a couple weeks. Staff did not think this was serious. I am really afraid. Thanks for your help
Please read this so you will know what I will be up against the end of January. This should answer all your questions.
Greg
Karen
with out bag but had problems while in hospital and since coming out only wish my doctor would have given me a bag people with bag fitted were going home after 5-7 days i still off work and have been told to expect another 2 months off thats 4 month in all .
Thank you for any help,
Tami
Thank you in advance for your help,
Linda
noreen
An epidural would not be appropriate for a procedure to that extent however I would ask about a spinal block, similar to an epidural but the medications are administered into two different locations. Epidural is only administered into the dura mater of the spine and the spinal block is administered in the subarachnoid space; allowing the medication to get into the CSF. Epidural is nice for a woman in labor but thats about it, a spinal provides loss of sensation to the entire body below the diaphragm. I really hope this helps but I am not an anesthesiologist or a doctor just a surgical technologist in training. God bless.
My doc is a great doc and told me that he has never lost a patient from this surgery and i am not going to be his first. Hope all goes well.
Is there any other medications I can take that is better for my system?
What are some foods that would be good for me?
Regards
R. Hornall
I think the original estimate was off. The colon is 5 feet. The polyps can be removed without removing any of the colon. I've been through 4 surgeries (just found out looking at a 3 resection) and 6 polyp removals.
Issue after colon resection .
Its difficult to plan outings cause I don't know what "today " will be like. Always have to be near a bathroom...and hope no one is using it when I go in there. And bless the person in the next stall...having to put up with the "sound effects and thunder coming from my stall". Its embarrassing, but what can one do? Sometimes I feel I have to explain why.
My family and friends tell me its ok to have these problems as its better than the alternative...DEATH!
Its hard to have to live life this way..but I am trying different things, foods, and activities and I am hoping to find a more normal life schedule.
constant pain akin to labor pain every day!! The doctor told me that I would feel much better after surgery. Instead he narrowed my rectum so that Now I need to have complete diarrhea to be able to void without pain. I was on pain meds for 13 years. I have decided to stop them and that has been even worse than living hell. I am half way there. Withdrawal is murder. Now, every time I have a Bm, I can feel my stitches pulling and it hurts a lot. I don't know how much more I can take!!
Because one of my family member is suffering so many complications after surgery and now main issue is she had undergone secondary suturing bt again after few days had so much ckear discharge and we came to know that again inside wound is open like abdomen or sheath as protein level is less in her