Simple mastectomy
Definition
Simple mastectomy is the surgical removal of one or both breasts. The adjacent lymph nodes and chest muscles are left intact. If a few lymph nodes are removed, the procedure is called an extended simple mastectomy. Breast-sparing techniques may be used to preserve the patient's breast skin and nipple, which is helpful in cosmetic breast reconstruction .
Purpose
Removal of a patient's breast is usually recommended when cancer is present in the breast or as a prophylactic when the patient has severe fibrocystic disease and a family history of breast cancer. The choice of a simple mastectomy may be determined by evaluating the size of the breast, the size of the cancerous mass, where the cancer is located, and whether any cancer cells have spread to adjacent lymph nodes or other parts of the body. If the cancer has not been contained within the breast, it calls for a modified radical mastectomy , which removes the entire breast and all of the adjacent lymph nodes. Only in extreme circumstances is a radical mastectomy, which also removes part of the chest wall, indicated.
A larger tumor usually is an indication of more advanced disease and will require more extensive surgery such as a simple mastectomy. In addition, if a woman has small breasts, the tumor may occupy more area within the contours of the breast, necessitating a simple mastectomy in order to remove all of the cancer.
Very rapidlygrowing tumors usually require the removal of all breast tissue. Cancers that have spread to such adjacent tissues as the chest wall or skin make simple mastectomy a good choice. Similarly, multiple sites of cancer within a breast require that the entire breast be removed. In addition, simple mastectomy is also recommended when cancer recurs in a breast that has already undergone a lumpectomy , which is a less invasive procedure that just removes the tumor and some surrounding tissue without removing the entire breast.
Sometimes, surgeons recommend simple mastectomy for women who are unable to undergo the adjuvant radiation therapy required after a lumpectomy. Radiation treatment is not indicated for pregnant women, those who have had previous therapeutic radiation in the chest area, and patients with collagen vascular diseases such as scleroderma or lupus. In these cases, simple mastectomy is the treatment of choice.
Finally, some women, with family histories of breast cancer and who test positive for a cancer-causing gene, choose to have one or both of their breasts removed as a preventative for future breast cancer. This procedure is highly controversial. Though prophylactic mastectomy reduces the occurrence of breast cancer by 90% in high-risk patients, it is not a foolproof method. There has been some incidence of cancer occurring after both breasts were removed.
Demographics
According to the American Cancer Society in 2003, it was estimated that more than 260,000 new cases of breast cancer in women would occur that year. New cases of breast cancer in men were expected to reach 1,300. Rates of incidence have increased since 1980, due in part to the aging of the population. During the 1990s, breast cancer incidence increased only in women age 50 and over.
For approximately 80% of women, the first indication of cancer is the discovery of a lump in the breast, found either by themselves in a monthly self-exam or by a partner or by a mammogram, a special x ray of the breast that looks for anomalies in the breast. Early detection of breast cancer means that smaller tumors are found that require lessintensive surgery and better treatment outcomes. Simple mastectomy has been the standard treatment of choice for breast cancer for the past 60 years. Newer breast-conserving surgery techniques have been gaining in acceptance since the mid-1980s. For larger hospitals, facilities in urban areas, and health care institutions with a cancer center or high cancer patient volume, these newer techniques are being utilized at a more rapid rate, especially on the East Coast.
Interestingly, though, the National Cancer Institute found in 2003 that American women were 21% more likely to have a mastectomy than their counterparts in the United Kingdom. Though breast-conserving procedures are available and have proven to be viable options, some physicians and women still think breast removal will also remove all of their risk of cancer recurrence. It is clear that treatment options for cancer are highly individual and often emotionally charged.
Description
Simple mastectomy is one of several types of surgical treatments for breast cancer. Some techniques are rarely used; others are quite common. These common surgical procedures include:
- Radical mastectomy is rarely used, and then only in cases where cancer cells have invaded the chest wall and the tumor is very large. The breast, muscles under the breast, and all of the lymph nodes are removed. This produces a large scar and severe disability to the arm nearest the removed breast.
- Modified radical mastectomy was the most common form of mastectomy until the 1980s. The breast is removed along with the lining over the chest muscle and all of the lymph nodes.
- Simple, sometimes called total, mastectomy has been the treatment of choice in the late 1980s and 1990s. Generally, only the breast is removed; though, sometimes, one or two lymph nodes may be removed as well.
- Partial mastectomy is used to remove the tumor, the lining over the chest muscle underneath the tumor, and a good portion of breast tissue, but not the entire breast. This is a good treatment choice for early stage cancers.
- Lumpectomy just removes the tumor and a small amount of tissue surrounding it. Some lymph nodes may be removed as well. This procedure is gaining acceptance among surgeons and patients alike.
Two other surgical procedures are variations on the simple mastectomy. The skin-sparing mastectomy is a new surgical procedure in which the surgeon makes an incision, sometimes called a keyhole incision, around the areola. The tumor and all breast tissue are removed, but the incision is smaller and scarring is minimal. About 90% of the skin is preserved and allows a cosmetic surgeon to perform breast reconstruction at the same time as the mastectomy. The subcutaneous mastectomy, or nipple-sparing mastectomy, preserves the skin and the nipple over the breast.
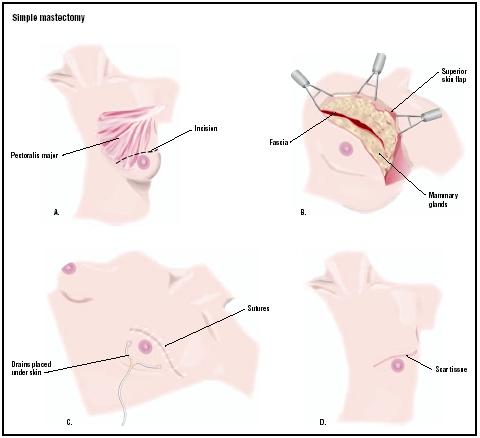
During a simple mastectomy, the surgeon makes a curved incision along one side of the breast and removes the tumor and all of the breast tissue. A few lymph nodes may be removed. The tumor, breast tissue, and any lymph nodes will be sent to the pathology lab for analysis. If the skin is cancer-free, it is sutured in place or used immediately for breast reconstruction. One or two drains will be put in place to remove fluid from the surgical area. Surgery takes from two to five hours; it is longer with breast reconstruction.
Breast reconstruction
Breast reconstruction, especially if it is begun at the same time as the simple mastectomy, can minimize the sense of loss that women feel when having a breast removed. Although there may be other smaller surgeries later to complete the breast reconstruction, there will not be a second major operation nor an additional scar.
If there is not enough skin left after the mastectomy, a balloon-type expander is put in place. In subsequent weeks, the expander is filled with larger amounts of saline (salt water) solution. When it has reached the appropriate size, the expander is removed and a permanent breast implant is installed.
If there is enough skin, an implant is installed immediately. In other instances, skin, fat, and muscle are removed from the patient's back or abdomen and repositioned on the chest wall to form a breast.
None of these reconstructions have nipples at first. Later, nipples are reconstructed in a separate surgery. Finally, the areola is tattooed in to make the reconstructed breast look natural.
Breast reconstruction does not prevent a potential recurrence of breast cancer.
Diagnosis/Preparation
If a mammogram has not been performed, it is usually ordered to verify the size of the lump the patient has reported. A biopsy of the suspicious lump and/or lymph nodes is usually ordered and sent to the pathology lab before surgery is discussed.
When a simple mastectomy has been determined, such preoperative tests as blood work, a chest x ray , and an electrocardiogram may be ordered. Blood-thinning medications such as aspirin should be stopped several days before the surgery date. The patient is also asked to refrain from eating or drinking the night before the operation.
At the hospital, the patient will sign a consent form, verifying that the surgeon has explained what the surgery is and what it is for. The patient will also meet with the anesthesiologist to discuss the patient's medical history and determine the choice of anesthesia.
Aftercare
If the procedure is performed as an outpatient surgery , the patient may go home the same day of the surgery. The length of the hospital stay for inpatient mastectomies ranges from one to two days. If breast reconstruction has taken place, the hospital stay may be longer.
The surgical drains will remain in place for five to seven days. Sponge baths will be necessary until the stitches are removed, usually in a week to 10 days. It is important to avoid overhead lifting, strenuous sports, and sexual intercourse for three to six weeks. After the surgical drains are removed, stretching exercises may be begun, though some physical therapists may start a patient on shoulder and arm mobility exercises while in the hospital.
Since breast removal is often emotionally traumatic for women, seeking out a support group is often helpful. Women in these groups offer practical advice about such matters as finding well-fitting bras and swimwear, and emotional support because they have been through the same experience.
Finally, for women who chose not to have breast reconstruction, it will be necessary to find the proper fitting breast prosthesis. Some are made of cloth, and others are made of silicone, which are created from a mold from the patient's other breast.
In some case, the patient may be required to undergo additional treatments such as radiation, chemotheraphy, or hormone therapy.
Risks
The risks involved with simple mastectomy are the same for any major surgery. There may, however, be a need for more extensive surgery once the surgeon examines the tumor, the tissues surrounding it, and the lymph nodes nearby. A biopsy of the lymph nodes is usually performed during surgery and a determination is made whether to remove them. Simple mastectomy usually has limited impact on range of motion of the arm nearest the breast that is removed, but physical therapy may still be necessary to restore complete movement.
There is also the risk of infection around the incision. When the lymph nodes are removed, lymphedema may also occur. This condition is a result of damage to the lymph system. The arm on the side nearest the affected breast may become swollen. It can either resolve itself or worsen.
As in any surgery, the risk of developing a blood clot after a mastectomy is a serious matter. All hospitals use a variety of techniques to prevent blood clots from forming. It is important for the patient to walk daily when at home.
Finally, there is the risk that not all cancer cells were removed. Further treatment may be necessary.
Normal results
The breast area will fully heal in three to four weeks. If the patient had breast reconstruction, it may take up to six weeks to recover fully. The patient should be able to participate in all of the activities she has engaged in before surgery. If breast reconstruction is done, the patient should realize that the new breast will not have the sensitivity of a normal breast. In addition, dealing with cancer emotionally may take time, especially if additional treatment is necessary.
Morbidity and mortality rates
Deaths due to breast cancer have declined by 1.4% each year between 1989 and 1995, and by 3.2% each year thereafter. The largest decreases have been among younger women, as a result of cancer education campaigns and early screening, which encourages more women to go to their physicians to be checked.
The five-year survival rate for cancers that were confined to the breast was 97% in 2003. For cancers that had spread to areas within the chest region, the rate was 78%, and it is only 23% for cancers occurring in other parts of the body after breast cancer treatment. The best survival rates were for early-stage tumors.
Two 20-year longitudinal studies concluded in 2002 indicated that the survival rate for patients with modified radical mastectomy (the removal of the entire breast and all lymph nodes) was no different from that of breast-conserving lumpectomy (the removal of the tumor alone). Implications of these studies suggest that the removal of the entire breast may not afford greater protection against future cancer than breast-conserving techniques. However, it should be noted that the majority of cancer recurrences occurred within the first five years for both those with mastectomies and those with lumpectomies.
Alternatives
Skin-sparing mastectomy, also called nipple-sparing mastectomy, is becoming a treatment of choice for women undergoing simple mastectomy. In this procedure, the skin of the breast, the areola, and the nipple are peeled back to remove the breast and its inherent tumor. Biopsies of the skin and nipple areas are performed immediately to assure that they do not have cancer cells in them. Then, a cosmetic surgeon performs a breast reconstruction at the same time as the mastectomy. The breast regains its normal contours once prostheses are inserted. Unfortunately, the nipple will lose its sensitivity and, of course, its function, since all underlying tissue has been removed. If cancer is found near the nipple, this procedure cannot be done.
See also Lumpectomy ; Modified radical mastectomy .
Resources
books
A Breast Cancer Journey. Atlanta: American Cancer Society, 2001.
periodicals
"American Women Still Having Too Many Mastectomies." Women's Health Weekly (February 6, 2003): 20.
Jancin, Bruce. "High U.S. Mastectomy Rate Is Cause for Concern." Family Practice News 33, no.2 (January 15, 2003): 31–32.
"Procedure Preserves Natural Appearance after Mastectomy." AORN Journal 77, no.1 (January 2003): 213–1.
Zepf, Bill. "Mastectomy vs. Less Invasive Surgery for Breast Cancer." American Family Physician 67, no.3 (February 1, 2003): 587.
organizations
American Cancer Society. (800) ACS-2345. http://www.cancer.org .
American Society of Plastic Surgeons. 444 E. Algonquin Rd., Arlington Heights, IL 60005. (888) 475-2784. http://www.plasticsurgery.org .
National Cancer Institute. 6116 Executive Boulevard, MSC8322, Suite 3036A, Bethesda, MD 20892-8322. (800) 422-6237. http://www.cancer.gov .
Janie Franz
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Simple mastectomy is performed by a general surgeon or a gynecological surgeon. If reconstructive breast surgery is to be done, a cosmetic surgeon performs it. Patients undergo simple mastectomies under general anesthesia as an inpatient in a hospital. There is a growing trend, due to reductions in insurance coverage and patient preference, to perform simple mastectomies without reconstructive breast surgery as outpatient procedures.
QUESTIONS TO ASK THE DOCTOR
- Why is this procedure necessary?
- How big is my tumor?
- Are there other breast-saving or less-invasive procedures for which I might be a candidate?
- What can I expect after surgery?
- Do you work with a cosmetic surgeon?
- Will I have to undergo radiation or chemotherapy after surgery?