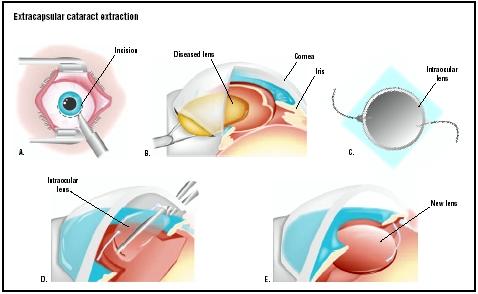
Extracapsular cataract extraction
Definition
Extracapsular cataract extraction (ECCE) is a category of eye surgery in which the lens of the eye is removed while the elastic capsule that covers the lens is left partially intact to allow implantation of an intraocular lens (IOL). This approach is contrasted with intracapsular cataract extraction (ICCE), an older procedure in which the surgeon removed the complete lens within its capsule and left the eye aphakic (without a lens). The patient's vision was corrected after intracapsular extraction by extremely thick eyeglasses or by contact lenses.
There are two major types of ECCE: manual expression, in which the lens is removed through an incision made in the cornea or the sclera of the eye; and phacoemulsification, in which the lens is broken into fragments inside the capsule by ultrasound energy and removed by aspiration.
Purpose
Historical background
The purpose of ECCE is to restore clear vision by removing a clouded or discolored lens and replacing it with an IOL. Cataract operations are among the oldest recorded surgical procedures; there are references to cataract surgery in the Code of Hammurabi in 1750 B . C . and in the treatises written around 600 B . C . by Susruta, a famous surgeon from India. In the ancient world, lenses damaged by cataracts were dislocated rather than removed in the strict sense; the surgeon used a lance to push the clouded lens backward into the vitreous body of the eye. This operation, known as couching, was standard practice until the mid-eighteenth century. Couching is still performed by some traditional healers in Africa and parts of Asia.
The first extracapsular extraction of a cataract was performed by a French surgeon named Jacques Daviel in 1753. Daviel removed the lens through a fairly long incision in the cornea of the eye. In 1865, the German ophthalmologist Albrecht von Graefe refined the operation by removing the lens through a much smaller linear incision in the sclera of the eye. After von Graefe, however, intracapsular extraction gradually became the favored method of cataract removal even though it left the patient without a lens inside the eye. The two inventions that made extracapsular extraction preferable again were the operating microscope and the intraocular lens. The first eye surgery performed with an operating microscope was done in Portland, Oregon, in 1948; in the same year, a British ophthalmologist named Harold Ridley implanted the first IOL in the eye of a cataract patient. Between 1948 and the 1980s, manual expression was the standard form of ECCE. Although phacoemulsification was first introduced in 1967, it was not widely accepted at first because it requires special techniques that take time for the surgeon to learn as well as expensive specialized equipment. As of 2003, phacoemulsification is now performed more often in the United States and Europe than "standard" ECCE. The manual expression technique, however, is still widely used in developing countries with large numbers of patients with eye disorders and limited hospital budgets.
The lens and cataract formation
To understand cataract surgery, it is helpful to have a basic description of the structure of the lens in the human eye. The lens, which is sometimes called the crystalline lens because it is transparent, is located immediately behind the iris. In humans, the lens is about 9 mm long and 4 mm wide. It consists of protein fibers and water, with the fibers arranged in a pattern that allows light to pass through the lens. There are three layers of cells in the lens: a central nucleus, which becomes denser and harder as a person ages; a cortex surrounding the nucleus, which contains cells that are metabolically active and continue to grow and divide; and a layer of cells between the cortex and the lens capsule known as the subcapsular epithelium.
Although a few people are born with cataracts or develop them in childhood, most cataracts are the result of the aging process. As people grow older, the protein fibers in the lens become denser, start to clump together, and form cloudy or opaque areas in the lens. Cataracts vary considerably in their speed of progression; they may develop in a few months or over a period of many years. Some people have cataracts that stop growing at an early stage of development and do not interfere with their vision. Although most people develop cataracts in both eyes, they do not usually progress at the same rate, so that the person has much better vision in one eye than in the other.
Ophthalmologists classify cataracts according to their location in the lens. It is possible for a person to have more than one type of cataract.
- Nuclear cataracts. Nuclear cataracts grow slowly over many years but can become very large and hard, which complicates their removal. They are sometimes called brunescent cataracts because they are characterized by deposits of brown pigment that give the lens an amber color. Nuclear cataracts are most commonly associated with age and with smoking as risk factors.
- Cortical cataracts. Cataracts in the cortex of the lens develop more rapidly than nuclear cataracts but remain softer and are easier to remove. They are thought to be caused by an increase in the water content of the lens. Risk factors for cortical cataracts include female sex and African or Caribbean heritage.
- Posterior subcapsular (PSC) cataracts. This type of cataract, which develops between the back of the lens and the lens capsule, is the softest and most rapidly growing type. PSC cataracts tend to scatter light at night and thus interfere with nighttime driving. Risk factors for PSC cataracts include diabetes and a history of treatment with steroid medications.
Demographics
Cataract extraction is one of the most frequently performed surgical procedures in industrialized countries. It is estimated that 300,000–400,000 cases of visually disabling cataracts occur each year in the United States alone, and that between 1 and 1.5 million cataract extractions are performed annually in the United States. This frequency reflects the importance of cataracts as a
major public health problem. The World Health Organization (WHO) estimated in 1997 that cataracts are responsible for 50% of cases of blindness around the world, or 19 million people. By 2020, that figure is expected to rise to 50 million. More recent publications estimate that 1.2% of the general population of Africa is blind, with cataracts responsible for 36% of these cases of blindness.
About one person in every 50 in the general American population will eventually have to have a cataract removed. It is difficult, however, to compare the rates of cataract formation among various subgroups because present published studies use a number of different grading systems for defining and detecting cataracts. In addition, the elderly are often under-represented in general population studies even though age is the greatest single risk factor for cataract development. Three recent research projects carried out in the United States, Australia, and England, respectively, reported that 50% of people over the age of 60 have some degree of cataract formation, with the figure rising to 100% for those over 80. As of 2003, little conclusive information is available regarding the incidence of cataracts in different racial and ethnic groups in the United States.
A variety of risk factors in addition to age have been associated with cataracts, but their precise significance is debated among researchers:
- Genetic factors. Twin studies show that the identical twin of a patient with a nuclear cataract has a 48% chance of developing one.
- Sex. Women are slightly more likely than men to develop cataracts. One American study found that 53.3% of women over 60 had nuclear cataracts compared to 49.7% of the men; 25.9% of the women had cortical cataracts versus 21.1% of the men.
- Exposure to ultraviolet radiation. Cortical cataracts are more likely to develop in people with frequent exposure to sunlight; however, nuclear cataracts are not related to sun exposure.
- Smoking. People who smoke more than 25 cigarettes per day are three times as likely as nonsmokers to develop nuclear or PSC cataracts. Smoking does not appear to be related to cortical cataracts.
- Alcohol consumption. Heavy drinking has been reported to increase the risk of developing all three types of cataracts.
- Diabetes. Patients with diabetes are at increased risk of developing all three types of cataracts.
- Use of steroid medications. PSC cataracts are known to be induced by steroids, even though they represent less than 10% of all cataracts.
- Socioeconomic status (SES). People with college or professional-school education have lower rates of cataract formation than people who did not finish high school, even attempting to correct for environmental and nutritional factors. There is, however, no obvious biochemical or medical explanation for this correlation, and some researchers treat it with caution.
- Chronic dehydration, diarrhea, and malnutrition. Studies carried out in India indicate that severe malnutrition or repeated episodes of diarrhea in childhood carry a three-to fourfold increase in risk of developing cataracts in later life. It is not yet known, however, whether this statistic would hold true for people in other countries.
Description
Conventional extracapsular cataract extraction
Although phacoemulsification has become the preferred method of extracapsular extraction for most cataracts in the United States since the 1990s, conventional or standard ECCE is considered less risky for patients with very hard cataracts or weak epithelial tissue in the cornea. The ultrasound vibrations that are used in phacoemulsification tend to stress the cornea.
A conventional extracapsular cataract extraction takes less than an hour to perform. After the area around the eye has been cleansed with antiseptic, sterile drapes are used to cover most of the patient's face. The patient is given either a local anesthetic to numb the tissues around the eye or a topical anesthetic to numb the eye itself. An eyelid holder is used to hold the eye open during the procedure. If the patient is very nervous, the doctor may administer a sedative intravenously.
After the anesthetic has taken effect, the surgeon makes an incision in the cornea at the point where the sclera and cornea meet. Although the typical length of a standard ECCE incision was 10–12 mm in the 1970s, the development of foldable acrylic IOLs has allowed many surgeons to work with incisions that are only 5–6 mm long. This variation is sometimes referred to as small-incision ECCE. After the incision is made, the surgeon makes a circular tear in the front of the lens capsule; this technique is known as capsulorrhexis. The surgeon then carefully opens the lens capsule and removes the hard nucleus of the lens by applying pressure with special instruments. After the nucleus has been expressed, the surgeon uses suction to remove the softer cortex of the lens. A special viscoelastic material is injected into the empty lens capsule to help it keep its shape while the surgeon inserts the IOL. After the intraocular lens has been placed in the correct position, the viscoelastic substance is removed and the incision is closed with two or three stitches.
Phacoemulsification
In phacoemulsification, the surgeon uses an ultra-sound probe inserted through the incision to break up the nucleus of the lens into smaller pieces. The newer technique offers the advantages of a smaller incision than standard ECCE, fewer or no stitches to close the incision, and a shorter recovery time for the patient. Its disadvantages are the need for specialized equipment and a steep learning curve for the surgeon. One study found that surgeons needed to perform about 150 cataract extractions using phacoemulsification before their complication rates fell to a baseline level.
Diagnosis/Preparation
Diagnosis
The diagnosis of cataract is usually made when the patient begins to notice changes in his or her vision and consults an eye specialist. In contrast to certain types of glaucoma, there is no pain associated with the development of cataracts. The specific changes in the patient's vision depend on the type and location of the cataract. Nuclear cataracts typically produce symptoms known as myopic shift (in nearsighted patients) and second sight (in farsighted patients). What these terms mean is that the nearsighted person becomes more nearsighted while the farsighted person's near vision improves to the point that there is less need for reading glasses. Cortical and posterior subcapsular cataracts typically reduce visual acuity; in addition, the patient may also complain of increased glare in bright daylight or glare from the headlights of oncoming cars at night.
Because visual disturbances may indicate glaucoma as well as cataracts, particularly in older adults, the examiner will first check the intraocular pressure (IOP) and the anterior chamber of the patient's eye. The examiner will also look closely at the patient's medical history and general present physical condition for indications of diabetes or other systemic disorders that affect cataract development. The next step in the diagnostic examination is a test of the patient's visual acuity for both near and far distances, commonly known as the Snellen test. If the patient has mentioned glare, the Snellen test will be conducted in a brightly lit room.
The examiner will then check the patient's eyes with a slit lamp in order to evaluate the location and size of the cataract. After the patient's eyes have been dilated with eye drops, the slit lamp can also be used to check the other structures of the eye for any indications of metabolic disorders or previous eye injury. Lastly, the examiner will use an ophthalmoscope to evaluate the condition of the optic nerve and retina at the back of the eye. The ophthalmoscope can also be used to detect the presence of very small cataracts.
Imaging studies of the eye (ultrasound, MRI, or CT scan) may be ordered if the doctor cannot see the back of the eye because of the size and density of the cataract.
Preparation
ECCE is almost always elective surgery—emergency removal of a cataract is performed only when the cataract is causing glaucoma or the eye is severely injured or infected. After the surgery has been scheduled, the patient will need to have special testing known as keratometry if an IOL is to be implanted. The testing, which is painless, is done to determine the strength of the IOL needed. The ophthalmologist measures the length of the patient's eyeball with ultrasound and the curvature of the cornea with a device called a keratometer. The measurements obtained by the keratometer are entered into a computer that calculates the correct power for the IOL.
The IOL is a substitute for the lens in the patient's eye, not for corrective lenses. If the patient was wearing eyeglasses or contact lenses before the cataract developed, he or she will continue to need them after the IOL is implanted. The lens prescription should be checked after surgery, however, as it is likely to need adjustment.
Aftercare
Patients can use their eyes after ECCE, although they should have a friend or relative drive them home after the procedure. The ophthalmologist will place some medications—usually steroids and antibiotics—in the operated eye before the patient leaves the office. Patients can go to work the next day, although the operated eye will take between three weeks and three months to heal completely. At the end of this period, they should have their regular eyeglasses checked to see if their lens prescription should be changed. Patients can carry out their normal activities within one to two days of surgery, with the exception of heavy lifting or extreme bending. Most ophthalmologists recommend that patients wear their eyeglasses during the day and tape an eye shield over the operated eye at night. They should wear sunglasses on bright days and avoid rubbing or bumping the operated eye. In addition, the ophthalmologist will prescribe eye drops for one to two weeks to prevent infection, manage pain, and reduce swelling. It is important for patients to use these eye drops exactly as directed.
Patients recovering from cataract surgery will be scheduled for frequent checkups in the first few weeks following ECCE. In most cases, the ophthalmologist will check the patient's eye the day after surgery and about once a week for the next several weeks.
About 25% of patients who have had a cataract removed by either extracapsular method will eventually develop clouding in the lens capsule that was left in place to hold the new IOL. This clouding, which is known as posterior capsular opacification or PCO, is not a new cataract but may still interfere with vision. It is thought to be caused by the growth of epithelial cells left behind after the lens was removed. PCO is treated by capsulotomy, which is a procedure in which the surgeon uses a laser to cut through the clouded part of the capsule.
Risks
The risks of extracapsular cataract extraction include:
- Edema (swelling) of the cornea.
- A rise in intraocular pressure (IOP).
- Uveitis. Uveitis refers to inflammation of the layer of eye tissue that includes the iris.
- Infection. Infection of the external eye may develop into endophthalmitis, or infection of the interior of the eye.
- Hyphema. Hyphema refers to the presence of blood inside the anterior chamber of the eye and is most common within the first two to three days after cataract surgery.
- Leaking or rupture of the incision.
- Retinal detachment or tear.
- Malpositioning of the IOL. This complication can be corrected by surgery.
- Cystoid macular edema (CME). The macula is a small yellowish depression on the retina that may be affected after cataract surgery by fluid collecting within the tissue layers. The patient typically experiences blurring or distortion of central vision. CME rarely causes loss of sight but may take between two and 15 months to resolve completely.
Normal results
Extracapsular cataract extraction is one of the safest and most successful procedures in contemporary eye surgery; about 95% of patients report that their vision is substantially improved after the operation. In the words of a British ophthalmologist, "The only obstacle lying between cataract sufferers and surgical cure is resource allocation."
Morbidity and mortality rates
Mortality as a direct result of cataract surgery is very rare. On the other hand, several studies have indicated that patients over the age of 50 who undergo cataract extraction have higher rates of mortality in the year following surgery than other patients in the same age group who have other types of elective surgery . Some researchers have interpreted these data to imply that cataracts related to the aging process reflect some kind of systemic weakness rather than a disorder limited to the eye.
About 23% of patients who have undergone cataract extraction have a postoperative complication. The majority of these, however, are not vision-threatening. The most common complication is swelling of the cornea (9.5%), followed by raised IOP (7.9%); uveitis (5.6%); leaking from the incision (1.2%); hyphema (1.1%); external eye infection (0.06%); endophthalmitis (0.03%); retinal detachment (0.03%); retinal tear (0.02%), and CME (0.017%). Of these complications, only endophthalmitis and retinal detachment or tear are considered potentially vision-threatening.
Standard ECCE and phacoemulsification have very similar success rates and complication rates when performed by surgeons of comparable skill and length of experience.
Alternatives
Medical treatment
As of 2003 there are no medications that can prevent or cure cataracts. Many ophthalmologists, however, recommend a well-balanced diet as beneficial to the eyes as well as the rest of the body, on the grounds that some studies suggest that poor nutritional status is a risk factor for cataract. While vitamin supplements do not prevent cataracts, there is some evidence that an adequate intake of vitamins A, C, and E helps to slow the rate of cataract progression. Elderly people who may be at risk of inadequate vitamin intake due to loss of appetite and other reasons may benefit from supplemental doses of these vitamins.
Watchful waiting
Not all cataracts need to be removed. A patient whose cataracts are not interfering with his or her normal activities and are progressing slowly may choose to postpone surgery indefinitely. It is important, however, to have periodic checkups to make sure that the cataract is not growing in size or density. In the recent past, surgeons often advised patients to put off surgical treatment until the cataract had "ripened," which meant that the patient had to wait until the cataract had caused significant vision loss and was interfering with reading, driving, and most daily activities. At present, ophthalmologists prefer to remove cataracts before they get to this stage because they are harder and consequently more difficult to remove. In addition, a rapidly growing cataract that is not treated surgically may lead to swelling of the lens, secondary glaucoma, and eventual blindness. In most cases, however, it is up to the patient to decide when the cataract is troublesome enough to schedule surgery.
Surgical alternatives
The major surgical alternative to ECCE is intracapsular cataract extraction, or ICCE. It is rarely performed at present in Europe and North America, but is still done in countries where operating microscopes and high-technology equipment are not always available. In ICCE, the surgeon makes an incision about 150 degrees of arc, or about half the circumference of the cornea, in order to extract the lens and its capsule in one piece. The surgeon then inserts a cryoprobe, which is an instrument for applying extreme cold to eye tissue. The cryoprobe is placed on the lens capsule, where it freezes into place. It is then used to slowly pull the capsule and lens together through the long incision around the cornea. Because of the length of the incision needed to perform ICCE and the pressure placed on the vitreous body, the procedure has a relatively high rate of complications. In addition, the recovery period is much longer than for standard ECCE or phacoemulsification.
Resources
books
"Cataract." Section 8, Chapter 97 in The Merck Manual of Diagnosis and Therapy , edited by Mark H. Beers, MD, and Robert Berkow, MD. Whitehouse Station, NJ: Merck Research Laboratories, 1999.
periodicals
Basti, S., P. Garg, and M. K. Reddy. "Posterior Capsule Dehiscence During Phacoemulsification and Manual Extracapsular Cataract Extraction: Comparison of Outcomes." Journal of Cataract and Refractive Surgery 29 (March 2003): 532-536.
Brown, Nicholas Phelps. "Medical Treatment of Cataract." Optometry Today (November 30, 2001): 28-32.
Grinbaum, A., M. Blumenthal, and E. Assia. "Comparison of Intraocular Pressure Profiles During Cataract Surgery by Phacoemulsification and Extracapsular Cataract Extraction." Ophthalmic Surgery, Lasers and Imaging 34 (May-June 2003): 182-186.
Guzek, J. P., and A. Ching. "Small-Incision Manual Extracapsular Cataract Surgery in Ghana, West Africa." Journal of Cataract and Refractive Surgery 29 (January 2003): 57-64.
Hammond, Chris. "The Epidemiology of Cataract." Optometry Today (February 9, 2001): 24-28.
Kalpadakis, P., et al. "A Comparison of Endophthalmitis After Phacoemulsification or Extracapsular Cataract Extraction in a Socio-Economically Deprived Environment: A Retrospective Analysis of 2,446 Patients." European Journal of Ophthalmology 12 (September-October 2002): 395-400.
Minassian, D. C., et al. "Extracapsular Cataract Extraction Compared with Small Incision Surgery by Phacoemulsification: A Randomised Trial." British Journal of Ophthalmology 85 (July 2001): 822-829.
Pesudovs, Konrad, and David B. Elliott. "The Evolution of Cataract Surgery." Optometry Today (October 19, 2001): 30-32.
Rowden, A., and R. Krishna. "Resident Cataract Surgical Training in United States Residency Programs." Journal of Cataract and Refractive Surgery 28 (December 2002): 2202-2205.
Thomas, R., T. Kuriakose, and R. George. "Towards Achieving Small-Incision Cataract Surgery 99.8% of the Time." Indian Journal of Ophthalmology 48 (June 2000): 145-151.
organizations
American Academy of Ophthalmology. P. O. Box 7424, San Francisco, CA 94120-7424. (415) 561-8500. http://www.aao.org .
American Optometric Association. 243 North Lindbergh Blvd., St. Louis, MO 63141. (314) 991-4100.
American Society of Cataract and Refractive Surgery (ASCRS). 4000 Legato Road, #850, Fairfax, VA 22033. (888) 949-6753. http://www.ascrs.org .
Canadian Ophthalmological Society (COS). 610-1525 Carling Avenue, Ottawa ON K1Z 8R9. http://www.eyesite.ca .
National Eye Institute. 2020 Vision Place, Bethesda, MD 20892-3655. (301) 496-5248. http://www.nei.nih.gov .
Prevent Blindness America. 500 East Remington Road, Schaumburg, IL 60173. (800) 331-2020. http://www.preventblindness.org .
Wills Eye Hospital. 840 Walnut Street, Philadelphia, PA 19107. (215) 928-3000. http://www.willseye.org .
other
D'Ocampo, Vicente Victor, and C. Stephen Foster. "Cataract, Senile." eMedicine July 18, 2002 [May 25, 2003]. http://www.emedicine.com/oph/topic49.htm .
National Eye Institute (NEI). Are You at Risk for Cataract? Bethesda, MD: NEI, 2001. NIH Publication No. 94-3463. National Eye Institute (NEI). Facts About Cataract . Bethesda, MD: NEI, 2001. NIH Publication No. 99-201.
Royal College of Ophthalmologists. Cataract Surgery Guidelines . London, UK: Royal College of Ophthalmologists, 2001.
Thomas, Ravi, and Thomas Kuriakose. "Surgical Techniques for a Good Outcome in Cataract Surgery: Personal Perspectives." Journal of Community Eye Health 13 (2000) [May 24, 2003]. http://www.jceh.co.uk/journal/35_4.asp .
Rebecca Frey, Ph.D.
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Cataract surgery is performed by ophthalmologists, who are physicians who have completed four to five years of specialized training following medical school in the medical and surgical treatment of eye disorders. Ophthalmology is one of 24 specialties recognized by the American Board of Medical Specialties.
If cataract surgery is being considered, it is a good idea to find out how many extracapsular extractions the surgeon performs each year. The greatest single factor in the success rate of ECCE procedures is not whether the surgeon performs a standard extraction or phacoemulsification, but the volume of operations that he or she performs. Surgeons who perform between 200 and 400 extracapsular extractions per year have higher rates of successful outcomes than those who perform fewer than 200.
Extracapsular cataract extractions are done as outpatient procedures, either in the ophthalmologist's office or in an ambulatory surgery center.
QUESTIONS TO ASK THE DOCTOR
- What type of cataract do I have and how fast is it developing?
- Would you recommend watchful waiting to see if surgery is necessary?
- How many cataract extractions do you perform each year, and what technique do you use?
- What is your success rate with cataract extractions?
Thank you for any further info you can send to me and answers to my questions.
Judith Watson
Dear Judith: well ur eye doc is right.if ur vision is improving with specs then no need of surgery at the moment.yup it is true for most of the ppl with a healthy retina that they wont be needing glasses for far vision but they may have to wear glasses for near for a condition known as Presbyopia.cataract surgery with Phaco wont help much to correct your astigmatism.
my email is mas1469@gmail.com
I am supposed to have cataract surgery. At my pre -op exam it was discovered that I have a clotting issue. It was determined that I have Factor X! deficiency. Is it necessary to have a plasma transfusion before having the surgery? My level indicates a severe deficiency. However, my history does not indicate any abnormal bleeding.
Now, 1 month after, she still complains of headaches and profuse tearing and pains in the eye. The IOL implant wasn't done because the surgeon said it didn't sit, but kept sinking as the zonules were not holding it, even though her iris was responding normally.
She also has been diagnosed with optic neuro-pathy.
What is the matter, why is she still experiencing all these discomforts? And should I be worried about the constant tearing that makes her look like she's crying??