Coronary stenting
Definition
A coronary stent is an artificial support device placed in the coronary artery to keep the vessel open after treatment for coronary artery disease. Also called atherosclerosis, coronary artery disease is a build-up of fatty matter and debris on the walls of the arteries. Over time, this buildup narrows the arteries and reduces blood supply to the heart.
The stent is usually a stainless steel mesh tube that is available in various sizes to match the size of the artery and hold it open after the blockage in the artery has been treated.
Purpose
The coronary stent is used to keep coronary arteries expanded, usually following a balloon angioplasty or other interventional procedure. Balloon angioplasty (also called percutaneous transluminal coronary angioplasty, or PTCA) and other interventional procedures are performed to open narrowed coronary arteries and improve blood flow to the heart. By forming a rigid support, the stent can prevent the vessel from reclosing (a process called restenosis) and reduce the need for coronary bypass surgery.
Demographics
According to the American Heart Association, 1,025,000 angioplasties were performed in the United States in 2000; of these, 561,000 were balloon angioplasties. There were 655,000 men and 370,000 women who had angioplasties in 2000. Stent placement is part of more than 70% of interventional procedures.
Description
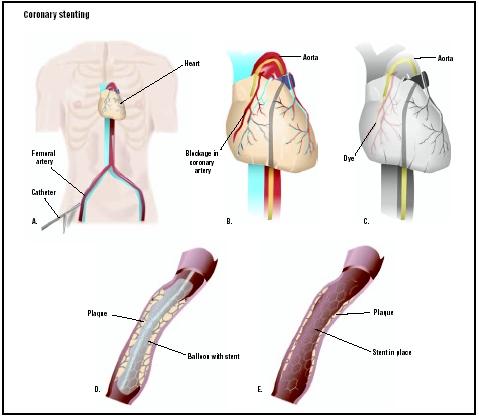
Coronary stenting usually follows balloon angioplasty. After the patient receives a local anesthetic to numb the area, a cardiac catheterization procedure is performed in which a long, narrow tube (catheter) is passed through a sheath placed within a small incision in the femoral artery in the upper thigh. Sometimes, the catheter is placed in an artery in the arm.
A catheter with a small balloon at the tip is guided to the point of narrowing in the coronary artery. Contrast material is injected through the catheter so the physician can view the site where the artery is narrowed on a special monitor. When the balloon catheter is positioned at the location of the blockage in the coronary artery, it is slowly inflated to widen that artery and compress the blockage or fatty area into the artery wall and stretch the artery open.
The stent is inserted into the artery with the balloon-tip catheter. When the stent is correctly positioned in the coronary artery, the balloon is inflated, expanding the stent against the walls of the coronary artery. The balloon catheter is deflated and removed, leaving the stent permanently in place to hold the coronary artery open.
Stents coated with drugs to decrease clotting or narrowing at the site are currently under investigation. These coated stents have significantly reduced restenosis rates—down to 3%—in some clinical studies. One coated stent brand, the Cordis CYPHER, became the first coated stent approved by the FDA in April 2003.
A cardiac angiography will follow to ensure that the stent is keeping the artery open.
Diagnosis/Preparation
Diagnosis
The diagnosis of coronary artery disease is made after the patient's medical history is carefully reviewed, a physical exam is performed and the patient's symptoms are evaluated. Tests used to diagnose coronary artery disease include:
- electrocardiogram
- stress tests
- cardiac catheterization
- imaging tests such as a chest x ray , echocardiography , or computed tomography (CT)
- blood tests to measure blood cholesterol, triglycerides, and other substances
Preparation
The patient should quit smoking or using tobacco products before the procedure, and needs to make the commitment to be a nonsmoker after the surgery. There are several smoking cessation programs available in the community. The patient can ask a health care provider for more information about quitting smoking.
The patient is usually instructed to take aspirin or another blood-thinning medication for several days before the procedure. Aspirin can help decrease the possibility of blood clots forming at the stent.
It is advisable for the patient to arrange for transportation home, because drowsiness may last several hours and driving is not permitted after the procedure.
After midnight the night before the procedure, the patient should not eat or drink anything.
The patient usually goes to the hospital the same day the procedure is scheduled, and should bring a list of current medications, allergies, and appropriate medical records upon admission to the hospital .
An intravenous needle will be inserted into a vein in the arm to deliver medications and fluids during the procedure. The catheter insertion site may be shaved. A sedative is given to make the patient drowsy and relaxed, but the patient will not be completely asleep during the procedure.
Aftercare
The procedure generally takes from 90 minutes to two hours to perform, but the preparation and recovery time add several hours to the overall procedure time. Although patients often go home the same day or the evening of the procedure, they should plan to stay at the hospital most of the day.
Recovery in the hospital
The patient is instructed to stay flat in bed without bending the legs so that the artery can heal from the insertion of the catheter. A stitch or collagen plug may be placed at the site of the catheter insertion to seal the wound and firm pressure may be applied to the area. A flat position is required for two to six hours after the procedure. A health care provider will help the patient get out of bed for the first time when the doctor approves it. The patient will be allowed to eat after he or she is able to get out of bed.
The patient is closely monitored during the recovery period. Vital signs and other parameters such as the heart's rhythm and electrical activity as well as oxygen and carbon dioxide levels in arterial blood are checked frequently. A catheter may be placed to drain urine during the recovery period.
A blood thinner may be given to the patient intravenously for the first few hours after the procedure to prevent clotting.
Recovery at home
Medications are prescribed to control pain. Minor chest discomfort is common after the procedure. However, the patient should notify the health care provider if severe chest, arm, or back discomfort is experienced. Some bleeding and bruising near the catheter insertion site are also common after the procedure. However, severe bleeding should be reported to a health care provider immediately. If bleeding occurs, the patient should contact 9-1-1 and lay down immediately. The dressing covering the area should be removed and firm pressure should be applied to the area until help arrives.
Ointments, lotions, and dressings should not be applied to the catheter insertion site unless specific instructions have been given.
Medications are prescribed to prevent unwanted blood clotting. Daily doses of aspirin or other anticoagulant medications are started after the procedure and are continued after the patient goes home.
The patient should not have any magnetic resonance imaging (MRI) tests for six months after the procedure, because the magnetic field may move the stent.
LIFESTYLE CHANGES. The patient needs to make several lifestyle changes after surgery, including:
- Quitting smoking. Smoking causes damage to blood vessels, increases the patient's blood pressure and heart rate, and decreases the amount of oxygen available in the blood.
- Managing weight. Maintaining a healthy weight by watching portion sizes and exercising is important. Being overweight increases the work of the heart.
- Participating in an exercise program. The exercise program is usually tailored for the patient, who will be encouraged to participate in a cardiac rehabilitation program supervised by exercise professionals.
- Making dietary changes. Patients should eat a lot of fruits, vegetables, grains, and non-fat or low-fat dairy products, and reduce fats to less than 30% of all calories. A diet low in cholesterol and vitamin K (to prevent interference with the anticoagulant medication) may be recommended.
- Taking medications as prescribed. Aspirin and other heart medications may be prescribed, and the patient may need to take these medications for life.
- Managing other health conditions such as diabetes or high blood pressure. Taking medications as prescribed and following the doctor's guidelines are very important ways for the patient to manage his or her health.
- Following up with health care providers. The patient needs to regularly see the physician to monitor his or her recovery and control risk factors. Routine stress testing is a part of the follow-up treatment to detect restenosis that may occur without symptoms.
Risks
Although coronary stents greatly reduce the risk of restenosis following balloon angioplasty, there is still some risk that the stented artery may close.
Serious complications are uncommon, but may include infection, damage to the heart or blood vessels, and blood clots. Anticlotting medication is given after stent placement to prevent the risk of blood clots. Less serious complications include bleeding, swelling, or bruising where the catheter was placed.
Normal results
The patient usually goes home the day or evening of the procedure, but sometimes an overnight stay in the hospital is necessary so monitoring can be continued. Patients should have someone to take them home after the procedure; driving is not recommended for at least 24 hours after the procedure.
Fatigue and weakness are common after the procedure. The patient should limit activities for the first two days after the procedure and can gradually resume normal activities by the end of the week.
For the first week after the procedure, pushing and pulling heavy objects (as in mowing the lawn) should be avoided, and lifting objects more than 20 lbs (9 kg) is not permitted. Stair climbing is permitted unless other instructions have been given.
Balloon angioplasty and the placement of a stent do not prevent coronary artery disease from recurring; therefore, lifestyle changes are strongly recommended and medications are prescribed to further reduce this risk.
Morbidity and mortality rates
Death is very rare (1%) as a result of the stent placement procedure.
Sometimes a blockage returns to the treated coronary artery (restenosis). If restenosis occurs, it usually happens within the first six months after the procedure. If the patient has previously experienced restenosis, there is an increased risk that it will recur. Repeat blockages can be treated with other interventional procedures; coronary artery bypass graft surgery may be needed.
Alternatives
All patients with coronary artery disease can help improve their condition by making lifestyle changes such as quitting smoking, losing weight if they are overweight, eating healthy foods, reducing blood cholesterol, exercising regularly, and controlling diabetes and high blood pressure.
All patients with coronary artery disease should be prescribed medications to treat their condition. Antiplatelet medications such as aspirin or clopidogrel (Plavix) are usually recommended. Medications may also be prescribed to lower lipoprotein levels, since elevated lipoprotein levels have been associated with an increased risk of cardiovascular problems.
Treatment with vitamin E is not recommended because it does not lower the rate of cardiovascular events in people with coronary artery disease. Although antioxidants such as vitamin C, beta-carotene, and probucol show promising results, they are not recommended for routine use. Treatment with folic acid and vitamins B 6 and B 12 lowers homocysteine levels (reducing the risk for cardiovascular problems), but more studies are needed to determine if lowered homocysteine levels correlate with a reduced rate of cardiovascular problems in treated patients.
Other interventional procedures used to open a blocked artery include rotoblation, brachytherapy, and atherectomy.
Coronary artery bypass graft surgery is a treatment option that is considered when medications and interventional therapies do not adequately treat coronary artery disease. During coronary artery bypass graft surgery, a blood vessel graft to restore normal blood flow to the heart is used to bypass one or more blocked coronary arteries. These grafts usually come from the patient's own arteries and veins located in the leg, arm, or chest.
Enhanced external counterpulsation (EECP) may be a treatment option for patients who are not candidates for interventional procedures or coronary artery bypass graft surgery. During EECP, a set of cuffs is wrapped around the patient's calves, thighs, and buttocks. These cuffs gently but firmly compress the blood vessels in the lower limbs to increase blood flow to the heart. The inflation and deflation of the cuffs are electronically synchronized with the heartbeat and blood pressure using electrocardiography and blood pressure monitors. EECP may encourage blood vessels to open small channels to eventually bypass blocked vessels and improve blood flow to the heart. Not all patients are candidates for this procedure, and treatments, lasting one to two hours, must be repeated about five times a week for up to seven weeks.
Resources
books
American Heart Association. "Considering Surgery or Other Interventions." In Guide to Heart Attack Treatment, Recovery, Prevention. New York: Time Books, 1996.
Barry, Frank. The Healthy Heart Formula: The Powerful, New, Commonsense Approach to Preventing and Reversing Heart Disease. New York: John Wiley & Sons, 1998.
Garratt, Kirk N., Guy S. Reeder, and David R. Holmes Jr. "Cardiac Catheterization and Angiography." In Mayo Clinic Practice of Cardiology, edited by Emilio R. Giuliani, et al. St. Louis: Mosby Publishing, 1996.
McGoon, Michael D., and Bernard J. Gersh. Mayo Clinic Heart Book: The Ultimate Guide to Heart Health, Second Edition. New York: William Morrow and Co., Inc., 2000.
Texas Heart Institute. Texas Heart Institute Heart Owner's Handbook. New York: John Wiley & Sons, 1995.
Topol, Eric J. Cleveland Clinic Heart Book: The Definitive Guide for the Entire Family from the Nation's Leading Heart Center. New York: Hyperion, 2000.
Trout, Darrell, and Ellen Welch. Surviving with Heart: Charge of Your Heart Care. Golden, CO: Fulcrum Publishing, 2002.
periodicals
Dangas, George, and Frank Keupper. "Restenosis: Repeat Narrowing of a Coronary Artery." Circulation 105 (2002): 2586–2587.
Michaels, Andrew D., and Kanu Chatterjee. "Angioplasty versus Bypass Surgery for Coronary Artery Disease." Circulation 106 (2002): e187–e190.
organizations
American College of Cardiology. Heart House. 9111 Old Georgetown Rd., Bethesda, MD 20814-1699. (800) 253-4636, ext. 694, or (301) 897-5400. http://www.acc.org .
American Heart Association. 7272 Greenville Ave. Dallas, TX 75231. (800) 242-8721 or (214) 373-6300. http://www.americanheart.org .
The Cleveland Clinic Heart Center, The Cleveland Clinic Foundation. 9500 Euclid Avenue, F25, Cleveland, Ohio, 44195. (800) 223-2273, ext. 46697, or (216) 444-6697. http://www.clevelandclinic.org/heartcenter .
National Heart, Lung and Blood Institute. National Institutes of Health. Building 1. 1 Center Dr., Bethesda, MD 20892. E-mail: NHLBIinfo@rover.nhlbi. http://www.nhlbi.nih.gov .
other
The Heart: An Online Exploration. The Franklin Institute Science Museum. 222 North 20th Street, Philadelphia, PA, 19103. (215) 448-1200. http://sln2.fi.edu/biosci/heart.html .
Heart Information Network. http://www.heartinfo.org .
HeartCenterOnline. http://www.heartcenteronline.com .
Cindy L. A. Jones, PhD
Angela M. Costello
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
A team of specialized heart doctors (cardiologists), nurses, and technicians trained in stent placement should perform this procedure. Stent placement usually takes place in the hospital setting in a special lab called the catheterization laboratory. It may also be performed in an intensive care unit , emergency room (such as for treatment of a heart attack), or other special procedure room.
QUESTIONS TO ASK THE DOCTOR
- Why is this procedure being performed?
- Should I take my medications the day of the procedure?
- Can I eat or drink the day of the procedure? If not, how long before the procedure should I stop eating or drinking?
- When can I drive after the procedure?
- What should I wear the day of the procedure?
- Will I be awake during the procedure?
- Will I have to stay in the hospital after the procedure?
- When can I resume my normal activities?
- When will I find out the results?
- What if the procedure was not successful?
- If I have had the procedure once, can I have it again to treat coronary artery disease?
- Will I have any pain or discomfort after the procedure? If so, how can I relieve this pain or discomfort?
- Are there any medications, foods, or activities I should avoid to prevent my symptoms from recurring?
Very concerned
The information is very valuable.
My husband had three stents five years ago. Last week he
had heart attack and the forth stent was put in. He is 67 years
old.
THANK YOU
MALCOLM
Remember when you bought a new car in 70's you had to get undercoating.
I read 1percent of people died, I read that a person was on a table n had a heart attack but survived? If my brother was at home n his crzy other didnt do anything to help him, n she killed before when she was younger n got away with it? Is there something we can do?
I hope you see this. I just went through pretty much everything I just read u posted
I already had a stint put in 7-8 years ago. About 2 yrs ago I began having chest pains and treated for high blood pressure The first of September I was hospitalized for a stroke Less than a week later after spending 8 days then less than 8 days later I had to go to another hospital because I kept falling out face first I admitted for blood pressure and afraid I'd had another stroke My first night in my heart rate dropped to 30. By the time it dropped to 19 a cardiologist decided to do artereragram through my leg and place a stent again He decided to place 3. Doing so he put one on top of another all the while I feel every thing including the rupture began internal bleeding while trying to communicate how bad my chest was hurting and how I couldn't breathe to be informed I was having a major heart attach by my nurse while they had to call another dr to go in my other leg to repair the damage done. I went straight to cicu and informed i would die without a blood transfusion. I received 5 pints of blood over 2 days. Four days later I received a pacemaker I didn't see that dr again and spent 13 days in the hospital that time. Almost 3 weeks later I still have alot of pain and there's still alot I can not do yet I worry how much longer I will experience these problems