Arthroplasty
Definition
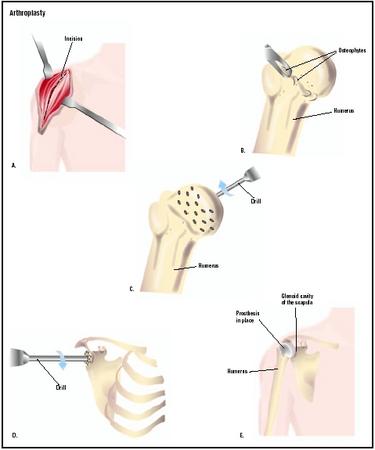
Arthroplasty is surgery performed to relieve pain and restore range of motion by realigning or reconstructing a dysfunctional joint.
Purpose
The goal of arthroplasty is to restore the function of a stiffened synovial joint and relieve pain. As a surgical procedure, it is usually performed when medical treatment has not improved function in the affected joint. There are two types of arthroplastic surgery: joint resection and interpositional reconstruction. Joint resection involves removing a portion of the bone from a stiffened joint, increasing the space between the bone and the socket to improve the range of motion. Scar tissue eventually fills the gap, narrowing joint space again. Pain is relieved and motion is restored, but the joint is less stable.
Interpositional reconstruction is surgery to reshape the joint and add a prosthetic disk between the two bones forming the joint. The prosthesis can be made of plastic, metal, ceramic material, or formed from such body tissue as skin, muscle, or fascia. When interpositional reconstruction fails, total joint replacement may be necessary. Joint replacement is also called total joint arthroplasty.
In recent years, joint replacement has become the operation of choice for most chronic knee and hip problems, particularly because of advances in the type and quality of prostheses (articifical joints). Elbow, shoulder, ankle, and finger joints are more likely to be treated with joint resection or interpositional reconstruction.
Arthroplasty is performed on people suffering from severe pain and disabling joint stiffness. Osteoarthritis (OA), a degenerative joint disease, is the most common condition causing joint destruction with pain and impaired movement. Other causes include rheumatoid arthritis (RA), hemophilia, synovitis, and rare bone diseases, which are all known to destroy cartilage. Joint resection, rather than joint replacement, is more likely to be performed on people with rheumatoid arthritis, especially when the elbow joint is involved. Joint replacement is usually reserved for older patients, because of the limited longevity of benefits. The younger the patient, the greater the reliance on medical treatment.
Demographics
The American Academy of Orthopaedic Surgeons reports that approximately 713,000 arthroplasty surgeries are performed annually in the United States. Of
Because the primary underlying condition in patients undergoing arthroplasty is osteoarthritis, a common cause for disability among older adults, the majority of patients undergoing this surgery fit the demographic profile for osteoarthritis. Osteoarthritis is the most common type of arthritis, with over twenty million people in all parts of the United States. Both men and women have the disease; under age 45 men are more often affected, though more women than men are affected after age 45. Younger people can have the disease after a joint injury. Arthroplasty is reserved for the most severely afflicted—approximately 3% of all patients with osteoarthritis, women more often than men. Two and one-half million people in the United States have rheumatoid arthritis, which can strike people of all ages. Very few have arthroplasty because this chronic crippling disease affects not only multiple joints but other parts of the body as well, including the immune system. Patients weakened by this disease are more subject to infection and less likely to enjoy positive surgical results.
Description
Arthroplasty is performed under general (affecting the entire body) or regional (numbing a specific area of the body, such as spinal block) anesthesia in a hospital, by an orthopedic surgeon. Although many hospitals and medical centers perform common types of joint surgery, orthopedic hospitals that specialize in joint surgery tend to have higher success rates than less specialized centers.
In joint resection, the surgeon makes an incision at the joint, then carefully removes the minimum amount of bone necessary to allow free motion. The more bone that remains, the more stable the joint. Ligament attachments are preserved as much as possible. In interpositional reconstruction, both bones of the joint are reshaped, and a disk of material is placed between the bones to prevent their rubbing together. Length of hospital stay depends on the joint affected; in the absence of complications, a typical stay is only a few days.
Diagnosis/Preparation
Significant disabling pain, deformity, and reduced quality of life are the primary indications for arthroscopic procedures. Patients at this stage of discomfort and disability will most likely have already been diagnosed with a form of arthritis. Pain and stiffness on weight-bearing joints are the major symptoms that patients report, though some people experience night pain as well. Other symptoms may include stiffness, swelling, and locking of the joint; and even the joint giving way, particularly when the knees or hips are affected. To determine the extent of disabling, the referring physician and/or the surgeon will likely ask about walking distance, sporting ability, the need for walking aids, and the ability to perform self-care tasks such as dressing and bathing. Besides evaluation of the joint itself and level of mobility, the clinical examination will include evaluation of the patient's general health, the condition of the ligaments and muscles around the affected joint, and also assessment of the patient's mental outlook and social circumstances to help develop the most effective postoperative rehabilitation plan. Diagnostic testing will typically include:
- x rays of the affected joint (and other joints as well)to determine loss of joint space and to differentiate between OA and RA
- imaging studies, such as computed tomography (Cat scans), magnetic resonance (MRI), and bone densitometry to assess bone loss or bone infection
- cardiac tests, such as electrocardiogram, to evaluate the heart and circulatory system
- blood tests to rule out infection and possibly to confirm arthritis
Prior to arthroplasty, standard preoperative blood and urine tests are performed to rule out such conditions as anemia and infection. If a patient has a history of bleeding, the surgeon may ask that clotting tests be performed. The patient will meet with the anesthesiologist to discuss any special conditions that may affect the administration of anesthesia. Surgery will not be performed if infection is present anywhere in the body or if the patient has certain heart or lung diseases. Smokers will be asked to stop smoking. Weight loss may also be recommended for overweight patients. If surgery involves deep tissue and muscle, such as total hip arthroplasty, the surgeon may order units of blood to be prepared in case transfusion is needed to replace blood lost during the surgery. Healthy patients may be asked to donate their own blood, which will be returned to them at the time of surgery (autologous transfusion). Certain pain medications may have to be discontinued in the weeks just prior to surgery.
Aftercare
Immediately after surgery, while still in the hospital, patients will be given pain medications for the recovery period and antibiotics to prevent infection. When patients are discharged after joint surgery, they must be careful not to overstress or destabilize the joint, requiring rest at home for a period of weeks. Physical therapy will begin immediately to improve strength and range of motion; it is the most important aid to recovery and may continue for several months. Activity may be resumed gradually, using devices if necessary, such as walkers or crutches, as recommended by the physical therapist. Lifestyle changes may include the use of special seating or sleeping surfaces, and employing home care assistance for help with shopping, cooking, and household tasks.
Risks
Joint resection and interpositional reconstruction do not always produce successful results, especially in patients with rheumatoid arthritis, a chronic inflammatory disease that may continue to narrow the joint space and accelerate the formation of scar tissue. Repeat surgery or total joint replacement may be necessary. As with any major surgery, there is always a risk of an allergic reaction to anesthesia, post-operative infection, or the formation of blood clots (thrombophlebitis) that may cause pain and swelling near the surgery site and travel through the veins to other parts of the body. A joint that has undergone surgery is less stable than a healthy joint and dislocation or loosening of the resected joint may occur, especially with inappropriate physical activity.
Normal results
Most patients enjoy an improved range of motion in the joint and relief from pain. Younger people may actually return to some form of low-impact sports activity. However, people who have degenerative or inflammatory diseases must understand that they will not suddenly have a normal joint, even while they will gain pain relief and improved function.
Morbidity and mortality rates
The number of deaths for all arthroplasty surgeries is less than 1%, with death more likely to occur among elderly patients and those with other serious medical conditions.
Alternatives
Pain management alone, particularly with the availability of more effective pain drugs that have fewer side effects, is the primary non-surgical option when the underlying diagnosis is a form of arthritis. Non-steroidal anti-inflammatory medications (NSAIDs) are commonly prescribed for arthritis sufferers, and people with RA are given certain drugs that suppress immune system activity, shown to be a factor in this type of arthritis. A range of nutritional supplements and vitamins are reported to offer health benefits to people with OA; among them, glucosamine and chondroitin sulfate have been shown to offer some relief for pain and stiffness. Weight loss is often recommended as well.
Because immobility of the affected joint can increase pain and stiffness, patients with joint disease are usually encouraged to continue some type of physical activity. Keeping the muscles strong through modest, non-weight-bearing exercise , such as stretching or swimming, is often recommended to help support the joint and maintain mobility. Various devices, such as braces or orthopedic shoes, may be recommended, as well as walking aids. Safety rails, special elevated toilet-seat extensions, bath and shower seats can make the patient more comfortable in daily life. Movement therapy, such as yoga, tai chi, and dance, may help maintain joint flexibility and slow chronic arthritis symptoms. Occupational therapy, massage therapy, and physiotherapy may help improve range of motion and overall comfort, as well as patient confidence.
Resources
books
"Joint Replacement." In Everything You Need to Know About Medical Treatments. Springhouse, PA: Springhouse Corp., 1996.
organizations
American Academy of Orthopaedic Surgeons(AAOS). 6300 North River Rd. Rosemont, Illinois 60018. (847) 823-7186. (800) 346-AAOS. Fax: (847) 823-8125. http://www.aaos.org .
Tish Davidson, A.M.
L. Lee Culvert
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
An orthopedic surgeon performs arthroplasty, including joint resection, interpositional reconstruction, and total joint arthroplasty (joint replacement). Orthopedic surgeons are board certified in their specialty and members of the American Academy of Orthopedic Surgeons (AAOS).
Orthopedic hospitals specialize in treating orthopedic conditions and performing orthopedic surgery . Although some orthopedic surgery may be performed in other hospitals and medical centers, better surgical results have been reported in the specialized centers.
QUESTIONS TO ASK THE DOCTOR
- Is surgery my only option? What alternatives might work?
- How many surgeries like mine have you performed?
- What can I do after surgery to improve the result and avoid more surgery?
- Will joint replacement be inevitable in time even if I have resection or reconstruction?
- What changes can I make in my lifestyle to slow the progress of arthritis?
Arthroplasty 2018 invites to be the Collaborator/Workshop/Exhibitor!!
Arthroplasty 2018 is an International Conference organized by Pulsus, welcomes all the eminent researchers and scholars around the globe to be the member of “11th International Conference on Arthroplasty†scheduled on September 24-25, 2018 at London, UK. The Objective of the Conference is to reach the Advancement in the Field of Arthroplasty by the global gathering and meeting of peoples from various diversities to share the knowledge by paper presentations, poster presentation and by the delivery of speech & lectures or as a Delegate in the research forum. Arthroplasty 2018 is eagerly waiting in addressing all the participants, scholars, researchers and industrial expects to make the gathering more successful.
Special Note: A group with 4-5 members can avail their special discounts in their group registration along with a complementary registration to experience the conference.
We cordially invite all the interested peoples and research forums to be a part of Arthroplasty 2018 at London by making your presence possible. Interested can also collaborate or make a partnership with Arthroplasty 2018. For more details about the event contact the email address: arthroplasty@pulsusmeet.org (or) arthroplasty@pulsusevents.org Visit: https://arthroplasty.cmesociety.com/