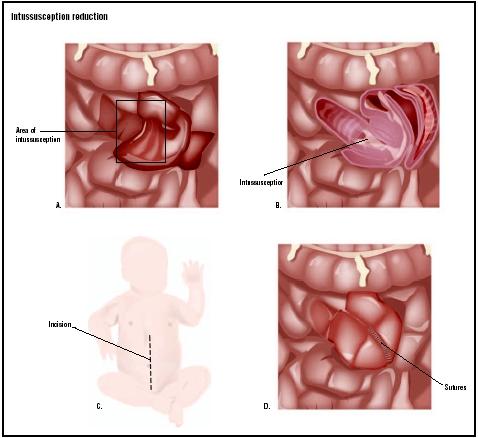
Intussusception reduction
Definition
Intussusception is a condition in which one portion of the intestine "telescopes" into or folds itself inside another portion. The term comes from two Latin words, intus , which means "inside" and suscipere , which means "to receive." The outer "receiving" portion of an intussusception is called the intussuscipiens; the part that has been received inside the intussuscipiens is called the intussusceptum. The result of an intussusception is that the bowel is obstructed and its blood supply gradually cut off. Surgery is sometimes necessary to relieve the obstruction.
Purpose
The purpose of an intussusception reduction is to prevent gangrene of the bowel, which may lead to perforation of the bowel, severe infection, and death.
The cause of intussusception is idiopathic in most children diagnosed with the condition (88–99%). Idiopathic means that the condition has developed spontaneously or that the cause is unknown. In the remaining 1–12% of child patients, certain conditions called lead points have been associated with intussusception. These lead points include cystic fibrosis; recent upper respiratory or gastrointestinal illness; congenital abnormalities of the digestive tract; benign or malignant tumors; chemotherapy; or the presence of foreign bodies.
In contrast to children, there is a lead point in 90% of adults diagnosed with intussusception.
Demographics
About 95% of all cases of intussusception occur in children. Children under two years of age are most likely to be affected by the condition; the average age at diagnosis is seven to eight months. Among children, the rate of intussusception is one to four per 1000. Conversely,
As of 2003, racial or ethnic differences do not appear to affect the occurrence of intussusception.
Description
Surgical correction of an intussusception is done with the patient under general anesthesia. The surgeon usually enters the abdominal cavity by way of a laparotomy, a large incision made through the abdominal wall. The intestines are examined until the intussusception is identified and brought through the incision for closer examination. The surgeon first attempts to reduce the intussusception by "milking" or applying gentle pressure to ease the intussusceptum out of the intussuscipiens; this technique is called manual reduction. If manual reduction is not successful, the surgeon may perform a resection of the intussusception. Resect means to remove part or all of a tissue or structure; resection of the intussusception, therefore, involves the removal of the area of the intestine that has prolapsed. The two cut ends of the intestine may then be reconnected with sutures or surgical staples; this reconnection is called an end-toend anastomosis.
More rarely, the segment of bowel that is removed is too large to accommodate an end-to-end anastomosis. These patients may require a temporary or permanent enterostomy. In this procedure, the surgeon creates an artificial opening in the abdomen wall called a stoma, and attaches the intestine to it. Waste then exits the body through the stoma and empties into a collection bag.
An alternative to the traditional abdominal incision is laparoscopy , a surgical procedure in which a laparoscope (a thin, lighted tube) and other instruments are inserted into the abdomen through small incisions. The internal operating field is then visualized on a video monitor that is connected to the scope. In some patients, the surgeon may perform a laparoscopy for abdominal exploration in place of a laparotomy. Laparoscopy is associated with speedier recoveries shorter hospital stays, and smaller surgical scars; on the other hand, however, it requires costly equipment and advanced training on the surgeon's part. In addition, it offers a relatively limited view of the operating field.
Diagnosis/Preparation
The diagnosis of intussusception is usually made after a complete physical examination , medical history, and series of imaging studies. In children, the pediatrician may suspect the diagnosis on the basis of such symptoms as abdominal pain, fever, vomiting, and "currant jelly" stools, which consist of blood-streaked mucus and pieces of the tissue that lines the intestine. When the doctor palpates (feels) the child's abdomen, he or she will typically find a sausage-shaped mass in the right lower quadrant of the abdomen. Diagnosis of intussusception in adults, however, is much more difficult, partly because the disorder is relatively rare in the adult population.
X rays may be taken of the abdomen with the patient lying down or sitting upright. Ultrasonography (an imaging technique that uses high-frequency sounds waves to visualize structures inside the body) and computed tomography (an imaging technique that uses x rays to produce two-dimensional cross-sections on a viewing screen) are also used to diagnose intussusception. A contrast enema is a diagnostic tool that has the potential to reduce the intussusception; during this procedure, x-ray photographs are taken of the intestines after a contrast material such as barium or air is introduced through the anus.
Children diagnosed with intussusception are started on intravenous (IV) fluids and nasogastric decompression (in which a flexible tube is inserted through the nose down to the stomach) in an effort to avoid surgery. An enema may also be given to the patient, as 40–90% of cases are successfully treated by this method. If these noninvasive treatments fail, surgery becomes necessary to relieve the obstruction.
There is some controversy among doctors about the usefulness of barium enemas in reducing intussusceptions in adults. In general, enemas are less successful in adults than in children, and surgical treatment should not be delayed.
Aftercare
After surgical treatment of an intussusception, the patient is given fluids intravenously until bowel function returns; he or she may then be allowed to resume a normal diet. Follow-up care may be indicated if the intussusception occurred as a result of a specific condition (e.g., cancerous tumors).
Risks
Complications associated with intussusception reduction include reactions to general anesthesia; perforation of the bowel; wound infection; urinary tract infection; excessive bleeding; and formation of adhesions (bands of scar tissue that form after surgery or injury to the abdomen).
Normal results
If intussusception is treated in a timely manner, most patients are expected to recover fully, retain normal bowel function, and have only a small chance of recurrence. The mortality rate is lowest among patients who are treated within the first 24 hours.
Morbidity and mortality rates
Intussusception recurs in approximately 1–4% of patients after surgery, compared to 5–10% after nonsurgical reduction. Adhesions form in up to 7% of patients who undergo surgical reduction. The rate of intussusception-related deaths in Western countries is less than 1%.
Alternatives
Such nonsurgical techniques as the administration of IV fluids, bowel decompression with a nasogastric tube, or a therapeutic enema are often successful in reducing intussusception. Patients whose symptoms point to bowel perforation or strangulation, however, require immediate surgery. If left untreated, gangrene of the bowel is almost always fatal.
Resources
books
"Congenital Anomalies: Gastrointestinal Defects." In The Merck Manual of Diagnosis and Therapy , edited by Mark H. Beers, MD, and Robert Berkow, MD. Whitehouse Station, NJ: Merck Research Laboratories, 1999.
Engum, Scott A. and Jay L. Grosfeld. "Pediatric Surgery: Intussusception." In Sabiston Textbook of Surgery . Philadelphia: W. B. Saunders Company, 2001.
Wyllie, Robert. "Ileus, Adhesions, Intussusception, and Closed-Loop Obstructions." In Nelson Textbook of Pediatrics , 16th ed. Philadelphia, PA: W. B. Saunders Company, 2000.
periodicals
Chahine, A. Alfred, MD. "Intussusception." eMedicine ,April 4, 2002 [cited May 4, 2003]. http://www.emedicine.com/PED/topic1208.htm .
Irish, Michael, MD. "Intussusception: Surgical Perspective." eMedicine , April 29, 2003 [cited May 4, 2003]. http://www.emedicine.com/PED/topic2972.htm .
Waseem, Muhammad and Orlando Perales. "Diagnosis: Intussusception." Pediatrics in Review 22, no. 4 (April 1, 2001): 135-140.
organizations
American Academy of Family Physicians. PO Box 11210, Shawnee Mission, KS 66207. (800) 274-2237. http://www.aafp.org .
American Academy of Pediatrics. 141 Northwest Point Blvd., Elk Grove Village, IL 60007-1098. (847) 434-4000. http://www.aap.org .
American College of Radiology. 1891 Preston White Dr., Reston, VA 20191-4397. (800) 227-5463. http://www.acr.org .
Stephanie Dionne Sherk
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Intussusception reduction is usually performed in a hospital operating room under general anesthesia. The operation may be performed by a general surgeon, a pediatric surgeon (in the case of pediatric intussusception), or a colorectal surgeon (a medical doctor who focuses on the surgical treatment of diseases of the colon, rectum, and anus).
QUESTIONS TO ASK THE DOCTOR
- What diagnostic tests will be needed to confirm the presence of an intussusception?
- Is there a lead point in this case?
- Can the intussusception be treated successfully without surgery?
- If resection becomes necessary, will an enterostomy be performed?
- How soon after surgery may normal diet and activities be resumed?
A 3-yr-old boy with intussuscetion undergoes a resection, but develops post-op adhesions. Since another surgery may produce more adhesions, what are other alternatives to help with recovery??
my daughter was operated for intussception at age of 15 months. she was operated twice for the same after pneumatically redution. Now she is 3.1 year old. till date she get obstruction and she is prone to loose stools. i want to know the reason behind this post surgical complications.
If anyone has any input it would be greatly appreciated.
I just got a diagnosis of intussusception yesterday. That was my after 3rd trip to the GI doc and after having a colonoscopy, endoscopy of stomach and duodenum, and a CT scan. I see my regular doctor every 3 months for another chronic illness and I have told him about my symptoms at every visit! Since the start of my more acute symptoms, 20 months ago, I've lost 60 pounds. Now that I've got the dumb DX, the GI guy tells me no surgeon will operate yet b/c my pain is intermittent and they think by the time they get me to an operating room the intussusception will have resolved itself (temporarily). I've got to wait till the pain gets worse and I start vomiting before they'll do surgery to fix it. At this point I'm so tired of dealing with the pain and tiredness of this added to my intractable pain from my other health issues that I'd kinda be okay with dying from complications of the surgery. I know that seems extreme, but it wears you down. And I've had to deal for a long time. You are extremely lucky to have gotten your DX so early in the process. Assuming you are otherwise very healthy, you will probably have a great outcome. All surgeries are risky and you've got to weigh the pro and cons based on your situation and what will benefit you the most… until, of course, you have that choice made for you by an emergency situation, or if you became unconscious and a loved one has to make the decision for you. Write up an advanced directive for yourself, so your wishes are followed once you decide on what you want. If you get the surgery, have lots of people help you with dealing with the kids, meals, housework, etc. Sometimes, if you are so inclined, church folk, or friends will help you with meals for the first few weeks of your recovery. I found lots of stuff on the Internet on this, so take advantage of it and your doctor, to get information. Good luck to you and your family. I know it's hard when kids are young. I've got 2 daughters who've had to live thru the journey and they're in their early twenties. They do survive. They're mad at me sometimes (ya know—they really struggle with understanding unless they experience it too), but they're doing okay.
I just wanted to put my story here, as many have before me. My intussusception blockage came fast and hit hard. I didn't feel any discomfort or pain days before this happened. When I heard I needed emergency surgery I was shocked. I honestly thought they had the wrong patient. The only thing looking back on that Saturday that should have alarmed me was the vomiting. Any vomit that resembles black tar with flakes; get to the er immediately.
please help me. i need help for medicien and food every day.
3 months later he went to ER but a small hospital. They diagnosed him with intususneption, with polyps and bowel obstruction. He was in the hospital for 6 days. He died within a month. He was a very healthy man. His reason of death was heart attack due to previous heart attack which is the upper right ventricle; and that it was hereditary. I did a lot of research. If the pain is like how my son discribes it then go to ER. Something triggered my sons heart attack. Hereditary or not- the problem was late diagnosis and i wished he asked for a blood test during his last visit to the doctor. He died 3 days after his last doctor visit. Google intususneption and show it to your doctor so they will consider. Ask to have the patient be hooked to a heart monitor no matter what age because according to autopsy he had a previous heart attack. Maybe the doctor could have seen that. He was a Police Officer. The training didnt give him a heart attack. It was after surgery. I think because his intestine telescoped and had stuck bowel, his blood was not as healthy to pump for his organs. His creatanine was high and Egfr is low so his kidney got affected. Im not a doctor, im the mom.