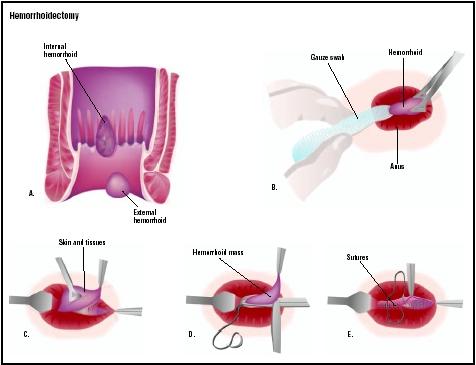
Hemorrhoidectomy
Definition
A hemorrhoidectomy is the surgical removal of a hemorrhoid, which is an enlarged, swollen and inflamed cluster
Purpose
The primary purpose of a hemorrhoidectomy is to relieve the symptoms associated with hemorrhoids that have not responded to more conservative treatments. These symptoms commonly include bleeding and pain. In some cases the hemorrhoid may protrude from the patient's anus. Less commonly, the patient may notice a discharge of mucus or have the feeling that they have not completely emptied the bowel after defecating. Hemorrhoids are usually treated with dietary and medical measures before surgery is recommended because they are not dangerous, and are only rarely a medical emergency. Many people have hemorrhoids that do not produce any symptoms at all.
As of 2003, inpatient hemorrhoidectomies are performed significantly less frequently than they were as recently as the 1970s. In 1974, there were 117 hospital hemorrhoidectomies performed per 100,000 people in the general United States population; this figure declined to 37 per 100,000 by 1987.
Demographics
Hemorrhoids are a fairly common problem among adults in the United States and Canada; it is estimated that ten million people in North America, or about 4% of the adult population, have hemorrhoids. About a third of these people seek medical treatment in an average year; nearly 1.5 million prescriptions are filled annually for medications to relieve the discomfort of hemorrhoids. Most patients with symptomatic hemorrhoids are between the ages of 45 and 65.
Risk factors for the development of symptomatic hemorrhoids include the following:
- hormonal changes associated with pregnancy and childbirth
- normal aging
- not getting enough fiber in the diet
- chronic diarrhea
- anal intercourse
- constipation resulting from medications, dehydration, or other causes
- sitting too long on the toilet
Hemorrhoids are categorized as either external or internal hemorrhoids. External hemorrhoids develop under the skin surrounding the anus; they may cause pain and bleeding when the vein in the hemorrhoid forms a clot. This is known as a thrombosed hemorrhoid. In addition, the piece of skin, known as a skin tag, that is left behind when a thrombosed hemorrhoid heals often causes problems for the patient's hygiene. Internal hemorrhoids develop inside the anus. They can cause pain when they prolapse (fall down toward the outside of the body) and cause the anal sphincter to go into spasm. They may bleed or release mucus that can cause irritation of the skin surrounding the anus. Lastly, internal hemorrhoids may become incarcerated or strangulated.
Description
There are several types of surgical procedures that can reduce hemorrhoids. Most surgical procedures in current use can be performed on an outpatient level or office visit under local anesthesia.
Rubber band ligation is a technique that works well with internal hemorrhoids that protrude outward with bowel movements. A small rubber band is tied over the hemorrhoid, which cuts off the blood supply. The hemorrhoid and the rubber band will fall off within a few days and the wound will usually heal in a period of one to two weeks. The procedure causes mild discomfort and bleeding. Another procedure, sclerotherapy, utilizes a chemical solution that is injected around the blood vessel to shrink the hemorrhoid. A third effective method is infrared coagulation, which uses a special device to shrink hemorrhoidal tissue by heating. Both injection and coagulation techniques can be effectively used to treat bleeding hemorrhoids that do not protrude. Some surgeons use a combination of rubber band ligation, sclerotherapy, and infrared coagulation; this combination has been reported to have a success rate of 90.5%.
Surgical resection (removal) of hemorrhoids is reserved for patients who do not respond to more conservative therapies and who have severe problems with external hemorrhoids or skin tags. Hemorrhoidectomies done with a laser do not appear to yield better results than those done with a scalpel. Both types of surgical resection can be performed with the patient under local anesthesia.
Diagnosis/Preparation
Diagnosis
Most patients with hemorrhoids are diagnosed because they notice blood on their toilet paper or in the toilet bowl after a bowel movement and consult their doctor. It is important for patients to visit the doctor whenever they notice bleeding from the rectum, because it may be a symptom of colorectal cancer or other serious disease of the digestive tract. In addition, such other symptoms in the anorectal region as itching, irritation, and pain may be caused by abscesses, fissures in the skin, bacterial infections, fistulae, and other disorders as well as hemorrhoids. The doctor will perform a digital examination of the patient's rectum in order to rule out these other possible causes.
Following the digital examination, the doctor will use an anoscope or sigmoidoscope in order to view the inside of the rectum and the lower part of the large intestine to check for internal hemorrhoids. The patient may be given a barium enema if the doctor suspects cancer of the colon; otherwise, imaging studies are not routinely performed in diagnosing hemorrhoids. In some cases, a laboratory test called a stool guaiac may be used to detect the presence of blood in stools.
Preparation
Patients who are scheduled for a surgical hemorrhoidectomy are given a sedative intravenously before the procedure. They are also given small-volume saline enemas to cleanse the rectal area and lower part of the large intestine. This preparation provides the surgeon with a clean operating field.
Aftercare
Patients may experience pain after surgery as the anus tightens and relaxes. The doctor may prescribe narcotics to relieve the pain. The patient should take stool softeners and attempt to avoid straining during both defecation and urination. Soaking in a warm bath can be comforting and may provide symptomatic relief. The total recovery period following a surgical hemorrhoidectomy is about two weeks.
Risks
As with other surgeries involving the use of a local anesthetic, risks associated with a hemorrhoidectomy include infection, bleeding, and an allergic reaction to the anesthetic. Risks that are specific to a hemorroidectomy include stenosis (narrowing) of the anus; recurrence of the hemorrhoid; fistula formation; and nonhealing wounds.
Normal results
Hemorrhoidectomies have a high rate of success; most patients have an uncomplicated recovery with no recurrence of the hemorrhoids. Complete recovery is typically expected with a maximum period of two weeks.
Morbidity and mortality rates
Rubber band ligation has a 30–50% recurrence rate within five to 10 years of the procedure whereas surgical resection of hemorrhoids has only a 5% recurrence rate. Well-trained surgeons report complications in fewer than 5% of their patients; these complications may include anal stenosis, recurrence of the hemorrhoid, fistula formation, bleeding, infection, and urinary retention.
Alternatives
Doctors recommend conservative therapies as the first line of treatment for either internal or external hemorrhoids. A nonsurgical treatment protocol generally includes drinking plenty of liquids; eating foods that are rich in fiber; sitting in a plain warm water bath for five to 10 minutes; applying anesthetic creams or witch hazel compresses; and using psyllium or other stool bulking agents. In patients with mild symptoms, these measures will usually decrease swelling and pain in about two to seven days. The amount of fiber in the diet can be increased by eating five servings of fruit and vegetables each day; replacing white bread with whole-grain bread and cereals; and eating raw rather than cooked vegetables.
Resources
books
"Hemorrhoids." Section 3, Chapter 35 in The Merck Manual of Diagnosis and Therapy , edited by Mark H. Beers, MD, and Robert Berkow, MD. Whitehouse Station, NJ: Merck Research Laboratories, 1999.
periodicals
Accarpio, G., F. Ballari, R. Puglisi, et al. "Outpatient Treatment of Hemorrhoids with a Combined Technique: Results in 7850 Cases." Techniques in Coloproctology 6 (December 2002): 195-196.
Peng, B. C., D. G. Jayne, and Y. H. Ho. "Randomized Trial of Rubber Band Ligation Vs. Stapled Hemorrhoidectomy for Prolapsed Piles." Diseases of the Colon and Rectum 46 (March 2003): 291-297.
Thornton, Scott, MD. "Hemorrhoids." eMedicine , July 16, 2002 [June 29, 2003]. http://www.emedicine.com/med/topic2821.htm .
organizations
American Gastroenterological Association. 4930 Del Ray Avenue, Bethesda, MD 20814. (301) 654-2055; Fax: (301) 652-3890. http://www.gastro.org .
American Society of Colon and Rectal Surgeons. 85 W. Algonquin Road, Suite 550, Arlington Heights, IL 60005. http://www.fascrs.org .
National Digestive Diseases Information Clearinghouse (NIDDC). 2 Information Way, Bethesda, MD 20892-3570. http://www.niddk.nih.gov .
other
National Digestive Diseases Information Clearinghouse (NDDIC). Hemorrhoids . Bethesda, MD: NDDIC, 2002. NIH Publication No. 02-3021. http://www.niddk.nih.gov/health/digest/pubs/hems/hemords.htm .
Laith Farid Gulli, M.D.,M.S.
Bilal Nasser, M.D.,M.S.
Nicole Mallory, M.S.,PA-C
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
A board certified general surgeon who has completed one additional year of advanced training in colon and rectal surgery performs the procedure. Specialists typically pass a board certification examination in the diagnosis and surgical treatment of diseases in the colon and rectum, and are certified by the American Board of Colon and Rectal Surgeons. Most hemorrhoidectomies can be performed in the surgeon's office, an outpatient clinic, or an ambulatory surgery center.
QUESTIONS TO ASK THE DOCTOR
- How many of your patients recover from hemorrhoids without undergoing surgery?
- How many hemorrhoidectomies have you performed?
- How many of your patients have reported complications from surgical resection of their hemorrhoids?
- What are the chances that the hemorrhoids will recur?
GOOD LUCK!!
Main recurrence off pain is from BMs (of course) but the pain meds (mine is Percocet) all bind the bowels, making it a catch-22. Today I'm biting the bullet and doing straight Tylenol. I find humor helpful. For instance I'm using pantie liners for pads and my wife had to explain to me that the sticky side goes on the underwear (I'm going to tell ALL my guy friends now).
Thanks
work i will never ever go through this procedure again,its worse than child birth.
good luck to all that choose this procedure,ITS PAINFUL.
Unfortunately the bleeding has started again and I seem to have painful lumps on the outside now. Not happy as I really don't want to go through this again.
I would appear to be one of the lucky ones who has had minimal, manageable (Vicodin) pain after surgery and very little problem with BM. I would emphasise what others write - I believe that the warm sitz baths and stool softeners are a must and really help speed the healing process along.
Patience is needed. I am nearly 5 weeks out and still have some leakage, but the pain now is only the itch and discomfort of (hopefully) healing surgery.
Please be aware of how serious this op is but also please take heart from the people who have come through without the dire results that some of these posts predict.
To ALL people here...this IS the most painful surgery I have EVER been through!
As one person stated,he questioned living it's self,that the pain level IS absolutly unbareable.I will tell you,he is NOT alone when saying that.
I am in the same boat as you are. I had the procedure done 3 weeks and 1 day ago. BMs are incredibly painful. It feels as though I am tearing apart. I have tried soaking several times a day over the last 3 weeks, using many different types of prescription creams and ointments and nothing has relieved the pain. I am at the point of holding in my BMs as I just can not deal with the pain. Hopefully someone has some advise that will help with this pain. It is by far the most painful procedure I have ever been through. I wish I had never done it.
If you really suffer and I mean that utterly miserable day after day soreness and pain that Hemorrhoids causes then I guess I'd say have the surgery. What you must remember is that pain is different for everyone. But I do think that the sites that say all should be well after 2 weeks are being hopeful at best. I'd double that at least. And dont go to gym for a while. Just take a gentle walk instead for a month or so. Best of luckj to anyone considering it.
I prepared for surgery just as I did for my first colonoscopy with a liquid diet the day before surgery and a complete purge using two 10oz bottles of magnesium citrate (one at noon, one at dinner 4pm). The next morning, one hour before heading to the hospital for surgery, I gave myself a Fleet enema. The surgeon didn't require this complete purge. My theory was that doing so would delay my first BM giving the surgical wound more time to settle down, and it would also ensure that no latent hard stuff would come down the tract and hurt me.
Surgery went well (I'm taking the doctor's word for that). The most pain I experienced in the hospital was when the IV sealed off and the liquid pain meds created a burning bubble under my skin. I was in the hospital for about 30 hours. The surgeon doesn't like to let his patients go home the same day -- and I'm glad about that.
I've been very strict about my high fiber diet (almost exclusively All Bran and Quick Oats) and lots of fluids -- about 32 oz (5 parts Gatorade, 1 part Cranberry juice for taste) every 4 hours since surgery. I've been taking 1 percocet every 3 hours and only some Ibuprofen periodically, and Colace twice daily.
Today (4 days after surgery) I had my first BM and immediately ramped up on the percocet. It was painful, but not like most descriptions on this and other forums. Just a bit of moaning, no howling or need to jump in the tub, etc. However, I'm now taking 1 percocet and 2 Ibuprofen every 2 hours. My stool was soft, but I've added Metamucil to the mix going forward -- it can't hurt. I've already had 4 significant BMs today. I quickly learned to not fight the BM. That is, most of my BM pain is in starting and stopping. So, once it starts, I keep the abdominal pressure on so that the flow will continue as long as possible, hopefully completing the BM in a single flow. That has worked very well since I tried it on the 2nd BM.
I'll be sticking to my diet of high fiber and lots of liquid until the BMs are essentially painfree. I'm guessing that may take another week.
Stitches are still there and I am still seeing bright, red blood.
My advice is that everyone take a long, hard look at their situation
before deciding to go with the surgery.
I have a very complicated situation because I also suffer from
severe migraines, lupus and fibromyalgia. As a result, I was kept
in the hospital 6 full days after surgery because it triggered a
horrible migraine. (I've put off the surgery to try all those other
alternative treatments for 3 years so my doctors and I did not enter
this surgery lightly.) I was given a DHE-45 treatment to ease the
migraine but was also given Vicodin (Norco) and Dilaudid while I
was in the hospital to ease the pain I felt ALL over my body including
the surgery site.
They sent me home with no painkillers for the first 24 hours due
to a mix-up, but every since then, I have been in pain at the surgery site
which keeps triggering my migraines. Ended up in the ER last week where, after
requesting the standard urine sample, the doctor on call tells me
there was blood in the urine, but don't worry because it was probably
just a hemorrhoid! I gave him the dirtiest look possible and calmly
explained to him that a hemorrhoidectomy is what I had JUST had so
the thought of another one being the cause of blood in my urine was
NOT what I wanted to hear.
Maybe things would have been different if I had gone home with the
painkillers as planned, but I can say that I truly still feel pain
and I will return to the surgeon on what will be exactly 1 month
feeling pretty much the same way I felt a few days after the surgery.
I just pray that it doesn't take much longer to heal.
1. drink lots and lots of water.
2. eliminate caffeine from your diet. I can't stress this enough. no coffee, no power drinks...
3. eliminate orange juice from your diet and replace with grapefruit juice w/2tbs olive oil
4. take psyllium fiber pills 2-3 times a day. No one gets enough fiber, even vegetarians
5. same as oj, tomatoes are acidic and should be avoided.
6. eat yogurt for healthy bacteria in your digestive system.
If all this fails, rubber band ligation is still way less painful than the roidectomy.
I'll post tomorrow how I feel before my gig.
1. drink lots and lots of water.
2. eliminate caffeine from your diet. I can't stress this enough. no coffee, no power drinks...
3. eliminate orange juice from your diet and replace with grapefruit juice w/2tbs olive oil
4. take psyllium fiber pills 2-3 times a day. No one gets enough fiber, even vegetarians
5. same as oj, tomatoes are acidic and should be avoided.
6. eat yogurt for healthy bacteria in your digestive system.
If all this fails, rubber band ligation is still way less painful than the roidectomy.
I'll post tomorrow how I feel before my gig.
HEMORRHOIDECTOMY SURGERY WAS WAY MORE ABOVE and BEYOND MORE PAINFUL THAN ANY OF THOSE SURGERIES!
Sitting is almost next to impossible, standing feels like to much pressure , laying on his side on an air matress helps some. BM's still extremely painful, and bleeding with clots. He'll be on the toilet and need to get in the tub immediately to wash off. Takes Hydrocodone , stool softners, metamucil, milk of magnesia, prune juice. He keeps a log on the counter to keep track of everything. When we left the Hospital that same day of the surgery, was given an appointment for a 2 week post op check (June 1) We have been back to the Doctor office 4 times now, with questions and concerns. Swelling, burning, bleeding, and what the hec are those new skin tags about ? ! Tags are so big they look like he was made a vagina ! Doctor says expect the bleeding yet for up to 2 more weeks. Return to work, MAYBE next week ! ? No after instructions came with the surgery, day by day basis, I guess ! The peeing was hard for the first 4 days, now it has finally got better. That leads us to believe the REAR will get better too ! We did not go on line, to search hemorrhoidectomy till AFTER the surgery. So reading these posts has helped us know that my husband is NOT the only one that is miserable. However, if we had read the posts and searched about the actual procedure, it may not have changed his mind, because the years of trying to push his grade 4 roids back in, were extremely painful, and bothersome , He still thinks he would have went ahead with the surgery. Hopefully in time, he will be able to tell you that he is glad he had it done, and all will be good. Until then THANKS for sharing ! If you are reading this, and deciding to have the surgery, YES it will be painful, but plan to allow at LEAST 3 - 4 weeks away from work, and healing slowly !! The bathtub is his best friend yet,He even is able to doze in the tub. We wish you all the BEST !
We just saw your post from July 5. We wrote the 5/27/11 post above yours. My husband wanted to let you know that he is getting better each day now. He is completely mobile again. Now, he has No regrets for doing the surgery. He felt like minimum of 3 weeks off, was best. His were inside and outside, Light bleeding, and stitches were still falling out at 5 weeks. He still takes stool softners regularly. It is REALLY a slow recovery. Take Care, and Best Wishes.
thank you
For most of the last 4 days, I've been either on the toilet, in the bathtub, or trying to sleep off the pain. I work from home, and I've been completely unable to work - that's quite a statement.
I've had frequent BMs - similar to what one commenter mentioned - small BM, clean up, and an uncontrollable urge would hit for another one...repeat the pattern over a couple of days. I've been yelling in pain during and after the BMs. I've cried as well - not a tear or two, but boo-hooing for several minutes.
I realize some folks have relatively minimal pain and recovery pretty quickly, but there are enough folks who have a much rougher go of it. I wish my doc would have have a LOT stronger words about the recovery when I was discussing the treatment options.
BTW, I did try infrared coagulation, but after treatment 2, I was in more pain than when I started. My doc said I was one of the few that IRC just wouldn't work for and that traditional surgery was my only course of action.
If you are researching this surgery, budget 2 weeks MINIMUM of down time - no work, no social engagements, nothing more physical than a very gentle walk. My employer is very upset with me because I did not set expectations what my actual recovery has been.
My surgery went pretty good, didn't feel the pain during the surgery because they put me to sleep.
After the surgery is when all hell broke loose , whenever I had the BM, it was excruciatingly painful.Urinating was tough the first couple of days.
This week's home recovery has been a challange.I have been taking two Percocet tablets every four hours for pain med's, I was still suffering with the pain during the BM.The bleeding and the swelling was pretty much common after the surgery.The sitz bath helps ease the pain, but doesn't get rid of it.I believe it is best to stay with liquids till this trauma is over, avoid taking solid foods till the first three weeks go by if possible.And stick with dietary fiber rich foods , fruits and vegetables to prevent hoids from coming back.
Close to my 6 weeks and all good.
On my first visit / exam with you , you had little bedside manner, but I have had good doctors that did not have this at first. This is not a big factor for me. During my visit, with you, I asked and you recommended a hemorrhoidectomy and said it was the only procedure for the size of my piles.
In asking you about time to plan for recovery, you seemed reluctant to state how long recovery would be. So, I asked, "5 days?, 5 to 7?" You suggested that was about right. So, my planning with work was to be ready to miss 1 week of work. I was optimistic as every surgery in the past the recovery has always been way quicker than expected. I am very well aware of pain and recovery from surgery. I can handle pain, expected pain, but guessed meds for 5 days or so would be enough.
You told me it was "the most painful surgery of all that you do", WHEN, *** AFTER *** I had the surgery. No, you are not alone, just read a forum like this one. Here is my biggest point, you need to raise above that level. You need to be the stand up physician that does not end up with someone like me that, if I had been briefed correctly, I would have likely chosen not to have the procedure done.
My other complaints include:
The very slim, written, post-surgery instructions you provide cover most, but some human overview of the pain meds and such should not be assumed. Most recoveries are not anywhere as complex. One lays around, washes in whatever way possible and takes pills as needed. Here, bowel movements create unbearable pain. Pill management is much more difficult. Baths are needed after every BM. Lidocain 5% ointment that I got by calling your line from another Doctor, (Chung?) ended up being very helpful.
While squirming in pain frequently and fearing bowel movements like torture, I looked on the web and found that most discussions of this procedure leave the patients wondering what kind of Docs like you that tell us 5 - 7 days for recovery. I think if you were honest and said 2 - 4 weeks, you might lose some patients, perhaps that is your alterior motive. During the call with Dr. Chung, he said he gets his patients to plan 3 weeks off of work. You could have spoke up if you thought I was in denial about 5 - 7 days, but you said that is about right.
In a few minutes you could have explained how to adjust stool softeners and made sure I had some 5% lidocain cream. On my first visit from pain about 5 days after surgery, you handed me a tube of 2% lidocain cream. WTF! - you had to know that 5% was available and could easily have written me a prescription. Seems to me that patient comfort should be higher on your list.
So, why would I write a letter like this. I wonder myself. I am pissed that you did not care enough to prepare me much better. I feel violated to have gone through so much pain that at minimum, I should have been forewarned would be there. If I was the litigious type, I would think about suing you, but that is not in my makeup. All I really want is for you to learn to be better at your next opportunity. You are a veteran. I am certain your surgical skills are great. Being a Doctor is a magical thing. Your lack of preparation and planning to make this experience as painless and at least to give me realistic expectations of how bad it could be is scandalous. The magic of being a physician is more than the technical side. On the human and forthright side, you need a ton of work. The pain one survives during the recovery is similar to torture. For the better part of the first two weeks, the pain I suffered kept me thinking that this is just wrong.
So, my only hope is that perhaps you can learn from this. That is all.
I now have to figure out for a final follow up if I should go to the other Dr. I mentioned. Dr. Chung, he almost sounded appalled when I described the 5 - 7 day recovery quote. He said he tells his patients to take 3 - 4 weeks off from work. Right on! Dr. Y (my doc) just needs to change his ways.
I am guessing that a doctor like this cannot respond to such an email as I noted above. Lawyers would want to keep any litigious documents to protect, just if there was a suit. I like my take, I just would feel so much better to at least have him acknowledge receipt of the above letter.
The email above was modified a bit, the gist is unchanged. I had to chop it down to under 4000 characters.
Would love any feedback. I chose not to display my email, but hope that I can come back here and see similar takes. As ugly as discussing the procedure, I lose my shame. I have already found two friend/acquaintances that are considering surgery. I think I saved them the torture that most of us have been through.
I now have to figure out for a final follow up if I should go to the other Dr. I mentioned. Dr. Chung, he almost sounded appalled when I described the 5 - 7 day recovery quote. He said he tells his patients to take 3 - 4 weeks off from work. Right on! Dr. Y (my doc) just needs to change his ways.
I am guessing that a doctor like this cannot respond to such an email as I noted above. Lawyers would want to keep any litigious documents to protect, just if there was a suit. I like my take, I just would feel so much better to at least have him acknowledge receipt of the above letter.
The email above was modified a bit, the gist is unchanged. I had to chop it down to under 4000 characters.
Would love any feedback. I chose not to display my email, but hope that I can come back here and see similar takes. As ugly as discussing the procedure, I lose my shame. I have already found two friend/acquaintances that are considering surgery. I think I saved them the torture that most of us have been through.
I had sensational pain and bleeding with uncomfortable slimy mucus at my anus. So my Dr. Said i had 3rd degree haemoriod.
the most painful thing in my life.
Anaestasia on my spinal cord made me feel no pain for op that lasted just 1hr. I heard it was painful but neva knew it was this extent, am 29yrs from Nigeria male, i decided to go for d op 2nd Dec 2011.
I'v been on liquid food, and fibric foods today 9th Dec, i urinated with scary pain d next day after d op and d jerking pain subsides as d day goes by. My ass now looks like a vagina lol with d stitch lumps but will stretch out sooner like my Dr said. Am taking vit c, tramadol, flygil, and oil parafin which seeps frm my ass lol. I am on sit warm salty saturated water bath, am praying to GOD that my 1st toileting not been painful. Am not having any swelling or bleeding. I wil be a lot betta by d Grace of GOD. I persistently confessed +vely to my antisipated 1st BM that it can NEVER pain me and back it up with drinking water, stool softner oil parafin, and eabric fruits am 1wk old after op.our
bodies differs with recovery.
Best wishes!
For those looking at undergoing the procedure, I will offer my advice. Sitz baths are amazing. It's hard to get up and take care of yourself when you feel this bad, but the effort will be rewarded. Do not "chase the pain". Stay on a good medication schedule. Ask your doctor to prescribe Lidocaine 5% ointment. Sit on an ice pack. Try to walk around to get some endorphins and prevent constipation. BMs are incredibly painful, so be prepared to start a Sitz bath right after you go. I use baby wipes instead of toilet paper.
I too, feel that this surgery wasn't explained as thoroughly as I would have liked. However, what's done is done and I'm looking forward to feeling better. On the other hand, I'm highly doubtful that two weeks is a sufficient period of time which to expect to be fully healed.
I welcome someonelse to give me his or her advice. Oh, and to the people on here talking about anal sex--what's WRONG with you? Doesn't your rear hurt enough???
THANK YOU
Fiber, water, stool softner...nothing seems to be making the BM easy...it's a sharp pain which I need to bear every morning...I am sad, worried and cursing my self for opting this surgery...any advise??!!
Try to avoid painkillers, because every painkiller has either paracetamol or ibuprofen or diclofenac, etc. and these cause severe bleeding and constipation in many people. U might want to stop the painkillers for 3-4 days (and bear the pain until then) but then u will see for yourself that bleeding reduces and STOPS. Do not take too much chemical laxatives as they can also cause swelling in rectum and bleeding and also swelling of lips,throat, etc. and cause more problems for BM since your bowel start depending upon them for making BM. You must must eat only boiled vegetables and fruits like dry figs, raddish, and try adding a little olive oil in ur diet as it helps to cleanse bowel easily. VERY IMPORTANT: Use KALONJI Oil with REAL PURE honey about 2 teaspoons daily (english name is Nigella sativa) it is the wonder herb known to Arabs and Indians to heal and finish any disease on earth. It has been used since times when there was no science of surgery more than thousands of years ago ! The difference will be visible usually within 3-4 days.
May GOD help reduce the sufferings of the sick
So best of luck everyone and take the responsibility yourself and the time to RESEARCH all options before you commit to surgery.
Blessings
Things that works for me:
- warm water applied (sits bath or standing in the bathtub with removable shower head) while urinating and after BM.
- clean the wound with warm water after BM to prevent from other infection.
- eat high fiber veggies/fruits for the 2 weeks.
- stay away from high protein meat (Dark meat, beef, ...)
- apply Vaseline at the anus before/after each BM. This helps stools for the ease of passage.
BTW. I was scheduling for 1week off as instructed by the doctor. However, I just extended for another week.
Good luck everyone!
please listen to me when i say this is a painful painful surgery. granted im almost only a week in, but people aren't kidding when they say they question living, and the pain is excrutiating. im not trying to scare anyone, just prepare you. try your best to remain in the hospital under their care for as long as possible, they have stronger pain meds that might help you get through the first extreme days. before the surgery, start a higher fiber liquid diet. prepare meals for your family ahead of time, and have someone there to take care of you while youre down.
im hoping tomorrow will be better, im so tired of hurting.
take care and i hope you all have an amazing day and feel wonderful very soon.
Have Been Living with this Pile for 2 Years.. took all kinds of Harbs..Tablets and Injections None seemed to work.. I had an Option for An Operation but when i taught about the Pain involved after the Operation i could'nt take the chance Not Until i found Out the Easy way to Kill and Stop the Pain.. First.. I stopped drinking or eaten anything that contains Sugar like Minerals... Alcoholic drinks... I had to stop Smoking as well... I eat More of Protain than Cabonhydrate foods.. Eat fruits and Drink lots of water... What gave me the total relief is Simple to get and Cheap to buy.. I Make Sure every Night Before i sleep i took 2 tablets of Bixacodine.. And i use blood capsules which contains Ginseng.. I took the Ginseng Blood capsule 1 3 times every Day.. 1 Morning 1 afternoon and 1 at Night hour.. Do this for 2 weeks and you will get your total relief of Pains... Make Sure you Avoid intake of Alcohol or Minerals.. If you want to get total relief of your Pile.. Thanks and God Bless..
Kelvin Dike
i just wanted to pop back in here to give an update on my recovery (had surgery 5/8/2012). things are going really well now. infact ive reached the 'itchy' phase, there isn't any real pain, just soreness and my rump itches, which means it is healing.
infact the pain is at such a low level im not taking any pain meds at all right now and haven't since yesterday. i still have not sat down as i don't feel my backside is ready for that yet. i also have moved back to super soft food like mashed potatoes for the mean time. i am trying to up my fiber intake by nibbling on 1/4 cup of fiber one cereal through today so it will go easy on my system.
i also went to the doctor yesterday and he said all was healing perfectly and tissue was still swollen. he said there will still be pain but each day i should continue to improve.
my bowel movements still hurt like heck, but the massive pain lasts for a short time then retreats some. This started yesterday, afterwards, I climb into the shower and use the shower stream to cleanse the area and direct warm water to that area. This helps soothe the pain some.
again, i will say the surgery is very painful, but i am total proof that it DOES get better. just try to stay on your stomach/side as much as possible. Soak in a CLEAN tub of warm water frequently (also make sure your feet are clean before getting in there), use a sitz bath that fits on the toilet to help with your bowel movements. It sounds totally gross, but it lessens the pain and lets things move a lot easier. Viva paper towels are super soft and assorbant as well as sturdy which helps with blotting dampness away from delecate areas, ive found they are softer than terry cloth washclothes. Whenever you can sleep- DO IT. Heck if you are able to, another idea would be to remain bottomless (without under garments)as much as possible to allow for air circulation.
Above all, try your best to relax and heal. Watch movies, read books, craft, write, whatever you enjoy. Keeping your mind occupied helps manage the pain as well. There are tons of movie sites online like netflix, amazon video and crackle. heck there is even YouTube to watch.
Take care all and I hope you all feel wonderful.
I will post again when i am able to sit again and the pain is completely gone so everyone can get an idea of healing periods and if i come up with other ideas to help out.
~Mindy
Many thanks for sharing your thoughts and experiences. No two individuals are the same and the amount of surgery varies of course from one person to another. Add to that, that a lot of people who go through the procedure without too much hassle will not have any horror stories to share here. So it's very difficult to know what a typical experience is. So please do not rely on this forum on trying to decide whether you should have the op or not. Know that the op should be fine and the post op recovery WILL be painful, and for some folk the worst pain they've experienced. But, no pain, no gain. and returning to work with a week off may be possible for smaller ops, but not for external piles imho.
So recovery tips in summary, from my experience:
1. Lots of fluid. This helps to avoid constipation.
2. Macrogol based stool softeners/osmotic laxatives (such as Movicol) which ensure that water is absorbed into the stools making them softer and easier to pass.
3. High fibre diet (I'm UK based and so I'm allowed to spell it like that!!) and reduce unnecessary solids that won't easily digest. Try more soups and less red meat, say. Remember, if you need to go less frequently for a BM you are increasing chances of healing between BMs AND thereby causing yourself less agony!
4. Consider soluble fibre supplements such as Benefiber powder, which is tasteless and totally soluble
5. Take prescribed analgesics (painkillers) round the clock and don't come off them too early. If you have had general anaesthetic, you will be benefiting from that initially which masks the true pain to come. Some of these drugs add to constipation and you may be tempted to leave them for that reason - forget that, you need them. The additional fibre should counterbalance that.
6. Using warm water to clean and relax muscles can help
7. Some people find a prescribed ointment called Diltiazem aids in the healing process. You should enquire about this from your doctor/surgeon
8. I was advised to walk, but was told this was to assist in avoiding constipation. I would say to rest and allow the wound to heal. As Mindy says, rest and allow the wound to heal. If you have an open wound from external piles, they are VERY raw at first, so gentle cleaning and air to breathe are good for them. If you have underwear that hospitals provide, you will see they are net/meshed based and allow good air flow whilst providing support. These are very useful.
Why does nobody get told all this good stuff BEFORE they have the surgery?!!
Best wishes all!
Shaf
I'm back for an update. If you look up a few posts, you will see I had my procedure done on 5/8/2012. Well, I want to let you know, I am sitting down on my chair now, it is a little uncomfortable but it works. I started driving again yesterday. Up until then it was a lot of pain when I tried. Also, bowel movements are almost completely pain-free.
I can do pretty much what I want now I believe. Granted, I am not going to over-do it because I don't want any pain again, but I am feeling quite well.
BTW- I did find out I had a prolapsed hemorrhoid and a few others.
Grace: About the swelling, I went through that as well. My doctor said it is normal and that area will be swollen for awhile. I was so scared the hemorrhoids had returned because of the swelling, but they didn't and everything is fine now. Hope you get well soon.
Alright, I am off of here. Take care all and I hope you all have speedy recoveries, feel amazing and no longer have to bow down to these pains in the rear.
~Mindy
Regard
Cindy
I have both internal and external. She said she would be using a "pain balloon" for afterwards to help with the pain. Apparently it is a catherer that goes on either side of the anus and when you are in pain you push a button and it injects pain medicine right to the source. It lasts for 4 days. Has anyone ever heard of this?! I can't find anything about it.
I just had a PPH surgery yesterday (9/13) for my stage 4 hemorrhoids. There was some discomfort for about 45 mins to an hour after the procedure. I could have left the hospital two hours after I woke up, but they wanted me to stay, just in case.
So, I left the hospital at around noon today - about 18 hours after the surgery, and went to a nice place for lunch.
I could have ridden a bicycle home from the hospital.
No pain,no discomfort, no bleeding, no weirdness, I feel just great.
I am a 50 y.o male, I just wish I had not put this thing off for so long.
I am not using any pain meds. The only problem I experienced was discovering how sensitive my system is to stool softeners. I had to go to the bathroom four times last night, so no more of that stuff, either.
I drove to the grocery store today, and took care of some household chores - just another uneventful, ordinary day.
I live in Istanbul, Turkey. I had my procedure done at Acıbadem Kadıkoy Hospital, by Nihat Yavuz.
I must say the difference in my quality of life has been immediate.
Not sure why they send you home same day. Pain killers only take the sharpest part of the edge off. I hope this is worth it when all is said and done, because right now, I'm pretty damn miserable. Impressive level of pain. I'd read some of the stories online, but I figured those were abnormal results...after all, I'm relatively healthy otherwise, I thought. Under 40, decent shape, good diet, above average tolerance for pain...boy was I wrong.
Night of the op, I thought my colon was going to explode. Couldn't pass gas or work up to a BM. I'm sore and bruised like the most popular boy at the prison prom. Spent most of today in hot bath water. That helps, but I can't sleep there. As disgusting as it is, I was finally able to have a BM while in the tub. But hell, at least it relieved a bit of the pressure. Was slightly less painful than the unpassable gas, but not by much. I now know what the phrase "tore him a new ass hole" would feel like, i think. And I could do without such terrible knowledge. Certainly broke new ground in the area of disgusting things my wife has had to help me with. Good thing we left the "...or worse" clause in the vows.
Just called doc requesting stronger meds...Percocet 5/325 were the initial scrip, doc just said I can take 2 at once, so hope that makes it better. Or at least leaves me unconscious for a few hours.
But yeah...painful is sort of an understatement.
surgeon has mentioned wanting to give me Botox injections to loosen scar tissue up and make things easier? I have also read quite a bit about dilating your rectum yourself to make the bowel movement process easier? Any suggestions??
The next morning I decided to drive myself 5 hours home, on the way the surgeon called and asked if I could be at the hospital at 115pm...I was half way home so I said sure! When I got there he took a look and said...WOW that is huge! Again thanks doc, he said it was an external thermbosed hemorrhoid about the side of a large grape. He asked me if I wanted to do it right there under local anth or schedule something else. I said this thing hurts, lets get it done! I was cautioned that the shots wouldn't be pleasant...it wasn't bad. They gave me 3 injections, one in the cheek, one next to the hemorrhoid, and one it it. After about a minute I couldn't feel a thing. The doc cut the clot out and the top of the hemorrhoid out...packed me up with gauze and taped me up. Only took about 15 minutes...I drove myself home and picked up one of those sitz baths. Got home around 4pm...when the shots wore off I had pain, but it wasn't anything worse than prior to surgery. I used the sitz before I went to bed...that helped. I took some advil that night and the next day. I have been taking stool softners and some fiber.
Instead of using the sitz, I have been using my jettub every morning after my BM, and than once when I get home from work, and once before bed. I went to work the day after the surgery ***note that was probably stupid*** but I figured it didn't hurt worse than prior to, and I went fishing so.
I used 3 x 3 gauze pads until Thursday for minor bleeding control, I also took some advil a few times. By today (Saturday day 5 after surgery) I was back in the woods hunting...climbing into my tree stand wasn't too bad, and I stayed there for 3 hours.
I don't know if it because where my hemorrhoid was located, my age (32), fitness, or just dumb luck but this wasn't too bad. Yes it hurts like a you know what but I got to say, much better at anypoint after than before. Honestly, I'm glad I didn't read this or I wouldn't have went for the surgery and that would have been a huge mistake.
Right now as I sit here, I couldn't tell you I feel anything wrong at day 6 after surgery. BM's don't really hurt much at all...(never did, even the first one after the surgery).
I missed one day of work..the day of the surgery, and that was because I was on vacation anyways.
Here are my experiences, and hopefully they can help someone. I had hemmoroidectomy & sphincterotomy exactly 2 months back to this date. The recovery has been very slow. I am still in pain after each BM every day. For the past week or so the pain is a bit bearable...it's about a 5 on a sclae of 1 - 10. My pathology indicated that there were 8 small to medium hemmoroids (internal as well as external) were removed covering an area of 3cm X 4cm.
My surgery was out patient surgery and was sent home an hour after the surgery. The surgery itself lasted 45min. I expected horrible pain anyway. First three days I had runs and made things worse. I became very weak and many times I couldnot feel lower part of my body due to pain. The pain level was a 9. There we different types of pains I felt through the next six weeks! Every time I ran my fingers across my lower back, I could feel different pain receptacles produce different pain...some cutting sensation, some stabbing, some throbbing, some ripping and so on. It's more like moving your fingers acorss a "piano of pain".
During first five weeks I only took Ibuprofen and Acetaminophen for pain. I refused to use serious narcotics like Hydrocodone, although my Dr prescribed that just in case. Three weeks back my Dr asked me to not to use even Ibuprofen. He simply asked me to "deal with it" and he expected my body to "get used to it". So no pain meds since. Every day after BM, I would suffer thru the pain from 6:30 am to 3 pm. After two months, I still feel pain after BM. There is a post surgery scar tissue that seem to swell up after BM every day and as along swelling stayed, the pain seem to be a constant issue.
For relief, this is what I did every day. After BM, I have been going for a walk for 30 min to an hour. That seem to relax my muscles and focus on other things than pain. When I get back from walk, I would either take a hot shower or bath. Wipe the area clean and apply Lidocaine ointment. (I think it is a steroid and acts like a local anesthetic) I also used Vaseline after each time I would clean the area. Drink 6 to 10 glasses of water. I ate scrambled eggs or omelette, oatmeal upma (look up on youtube on how to make it), lots of veggies, spinach. Ate a carrot three to four times a day. This gave me enough fiber for my next BM. Refused to eat meat or chicken...for some reason the days when I ate any meat I had painful BMs. But sauteed fish fillet worked very well. I also have been using a hot water bottle when I lay down or sleep at night...which definitely seem to provide a good relief from pain. Most importantly surround yourself with loved ones who are willing to help you when you need them. I owe it my wife and three kids who have been there every time I needed them.
Hopefully I am close to getting my health back and kick this pain to the curb permanently. Good luck with those of you planning this surgery and wish a speedy recovery to those who have already gone thru it.
So far this morning I'm still in quite some pain, but fine enough to write this. I'm not out of the woods yet, but so far i can say that it's not as bad as I had anticipated. If one has had piles that are bad enough and for long enough to need surgery, then one is already well used to pain so it hardly makes a difference.
I kow I will still be in for a few more surprises regarding the healing process. I will concentrate on gettign my liquid diet and papaya. They help soften your stool also. Until i am completely healed, i can say this with finality. Forget what the doctor say -- think about the bad experiences people suffered in getting the procedure done and weigh it against your choice. At the end of the day -- it will be your pain and not the pain of someone who'll say everything is going to be ok.
The flight or fight scenario, in my case the run to the loo option. This was never discussed before surgery which made my recovery slow and painful.
I'm sure there are a lot of people that eat a normal diet that are not constipated but still get hemorroids.
What made my recovery slower than expected was everytime I knew a BM was coming I would tense up. The urge to push was overwhelming to the point I couldn't stop, this of course caused damaged that took extra to heal.
The trick is to eat a high fibre diet, drink plenty of water,ease back on the meds and salt baths.
Oh! the most important thing is to remain calm and in control during the visit to the loo.
Good luck.
I have heard from different people that have gone thought this experience and it varies greatly.
The recovery process/pain will depend on the amount of surgery done.
The first BM after surgery is when you will need to remain calm and in control.
I was talking stool softening medication that helped.
It's day 11 for me and I am returning to work tomorrow, light duties only.
Remember it will only get better from here.
Santo
Anyway the op and post initial op pain is the easy part, the hard and TERRIBLE part of the operation is the BM or lack of it, I managed 3 tiny stools 3 days after op, since then nothing, but I am getting constant urge to go all that comes is wind and fluid, (very little though) I have followed all the advice with fibre diet, drink lots of water, soften stools, etc etc but still can't get BM
and each visit to the toilet is agony that last for hours afterwords, the pain relief available does not work, I tried a tens machine last night and finally managed to sleep a few hours though not totally pain free, I'd say about 30% extra pain relief with the tens, to be honest 10% more is heaven 30% feels like just having the piles back and is bearable.
I have leakage every time I pass wind, and this is so demoralising but very little blood loss and it is diluted.
At this time wishing I'd not had this done, hoping this wish change as the days go by,
When passing motion, do not sit but rather bend knees slightly from standing position. This is actually an easier way to do it.
What most people don't tell you about fibre diet is how some fibre can make it worse.
Be careful to choose only the finest fibre u can think of. Even some fibre solutions with husks etc make it worse. You will actually br able to feel the tiniest
Piece of passing the anus. Every one is a needle. Btw I had internal and external and multiple roids.
No oily food... Will make it worse. No starchy food too - spells trouble.
When having any food, make sure u chew em and mash em up well. This will help.
Sitz is also a great help. U will get tired sitting there but necessary.
2 weeks recovery? Maybe for the least of roids but for me, at least a month b4 any light work was possible.
Just remember again, the most crucial post ops pain management in all this is having soft stool which means U must experiment with the food that works for u
I am not a colorectal or general surgeon, but I am a surgeon in a different field. I thought I would have this down, no problem. Let me tell you that hemorrhoidectomy has long been known within the field of medicine to be one of the most painful recoveries for recovery. There are some that say the treatment is worse than the disease. That thinking is 100% correct as I am a pretty tough woman- no problem with natural labor, stage 4 endometriosis and multiple surgeries to correct that, horrific care accident and facial surgeries which were none too fun for recovery.
I am now day 7 after this procedure. I had this done due to lifelong hemorrhoids that worsened with childbirth and thrombosis of some internal prolapsing ones 3 times at the end of pregnancy and right after. I was sadly, induced at 40 weeks due to uncontrollable pain and had an I&D of the clot just before delivery room (in the LDR) and the day after delivery due to recurrence of the clot. Two weeks later I had a third and an I&D in the colorectal's doctor's procedure room. I then had banding done 6 week post-partum, which is not comfortable by any means and the GI physician would only do up to 2 at the time due to pain. I used only Tylenol because I was breastfeeding which did not help the experience. It has been two years since then. About six months ago, I noticed recurrence of the internal prolapsing hemorrhoids. Thursday evening I suddenly had recurrence of clot and immediately called my surgeon. He called in some pain medicine and I had some Marcaine (local anesthetic) on hand which made it so I could sit and sleep.
Friday I saw him in the office and we discussed that with failed banding, my young age, and desire to have one more baby, it was time to bite the bullet and have it done. Here is what I have learned and my survival guide for getting through this.
1. If at all possible, do a bowel prep or an enema prior to the surgery. If pain is a limiting factor, ask your surgeon about at least doing an enema in the OR.
2. If you have low pain tolerance, staying overnight is not a bad idea.
3. Most surgeons are already doing this, but before your surgery bed, plead and barter for injection of a local long-acting anesthetic (Marcaine is great). A Marcaine after surgery helps to control bleeding and will keep you numb for most of overnight of the first night after surgery.
4. Do not overcommit yourself after the surgery. Plan on staying recumbent for about a week. Gravity- standing, sitting, bending all increase swelling at the site. Since that swelling has impact on your pain and ability to have a BM, this is very important. Interposing 20 minutes of an ice pack and 20 minutes of heat by heating pad on a medium setting will help get swelling down.
5. Try very hard not to get constipated!!! This is almost impossible. I had to return post-op day #6 to be dismipacted, but I also have a rectocele which greatly contributed to being unable to pass my first BM. Surgeons do not always evaluate for this, so if you are a woman and have ever had to use a finger in the vagina to help evacuate stool, you probably have a (cont...)
rectocele. You should discuss with your doctor any individual issues that will pose a challenge to recovery. Other ways that are musts to avoid constipation: use around the clock non-steroidals (ibupfrofen, aleve, diclofenac, etc) instead of narcotics as a mainstay for pain. Take the non-steroidal at the time interval prescribed, whether you are having pain or not. Use narcotics for breakthrough only (which you will use plenty). Hydrate yourself incredibly well. Have some level of mild exercise daily (a short walk as a rest from lying down all day). Walking will help the bowels move. Eat all high fiber until you are healed. Use daily or twice daily fiber additive like Metamucil. Colace (stool softener) to its maximum dose is recommended (ask your doctor how much you can safely take.) For those with bowels very sensitive to narcotics (like mine, as in instant constipation) may also want to consider taking a small amount of a bowel prep daily as a laxative. Ask your doctor what is recommended. For me, I am now taking 8 0z of Go Lytely daily to keep my bowels watery until I am healed!
Best of luck. This is a very painful recovery process so be sure that you have exercised all forms of more conservative therapy. The post-operative pain you will experience will also depend on the type of hemorroidectomy done (open versus closed, stapled), +/ sphincterotomy, so be sure you discuss all of these details with your doctor to know what you are getting into..
Happy healing!
I never really siffered with pain, just a discomfort and had tried rubber band ligation to no affect.
I had surgery five days ago. Yes you do get immense pain that first night and for the next couple of days. Now it only hurts when I have a bowel movement. I am still passing a little blood but only when on the toilet and a slight difficulty in urination as my bowel seems to 'spasm' when trying to pass water so it is a bit painful.
The secret for me for to have, again, a good fibrous diet and TAKE YOUR MEDICATION REGULARLY. Don't wait for the pain to come on before you take it, but take it religiously as directed even if there is no pain. The other thing I did was to make sure I had a nice warm bath run before I went to the toilet so that as soon as I was done I could hop straight in it.
I went into a Surgical Short Stay ward in the hospital here in the UK, was kept in for about 3 hours post operation and sent home with Codeine, Ibuprofen, Paracetamol, Lignocaine (to numb the area around the rectum after a bowel movement and bath), antibiotics and Lactulose.
The short (but painful) duration of the pain for a few days is absolutely worth going through for the quality of life afterwards.
I'm a 35 year-old male, average height and weight with no past medical history if this helps.
itching that began last night - I might lose my mind!!!
They immediately admitted me and scheduled my surgery for the next day. I was given Morphine which made the pain manageable. I was feeling better and thought relief would soon come. I don't remember the surgery, I was put under. I was given something right after surgery which made me stop breathing a couple of times. By the time I got to my room, I wasn't feeling too bad. The doctor used a long lasting local which allowed me to sleep some through the night. I had trouble urinating but could get some out with minor straining. I had no appetite, just drank alot of liquids. My colon surgeon had the worst bed-side attitude, most of the nurses and ward doctor did. They always reminded me of this being an Out-Patient procedure. Well, I'm sorry to say I don't agree with that at all. Anyways, they allowed me to stay for 1 day, still no appetite, still a struggle to urinate, and no BM yet. They practically booted me out, even while I was getting dressed, I almost passed out, got all dizzy, dripping with sweat. The nurse called the ward doctor and she said it was just because I was lying in bed all day. Anyways, I got dressed and the nurse practically was running me out in the wheel chair. I was given some prescriptions for pain, mineral oil and was told to start taking Metamucil.
I was in so much pain and practically lived in the bathtub for the first 3 days, started a liquid diet. I had alot of gas, leakage and had a good BM while in the tub(could stop it- very runny) the 2nd day. The pain with the BM was manageable because it was so loose I guess, but alot of burning. The easiest way for me to urinate was in the tub. On the 3rd day I felt the need for another BM and decided to try the toilet. What a mistake that was, the pain was so excruciating I almost passed out. It was still soft, kinda pancake batter consistency. I immediately jumped in the tub and soaked in cold water which helped with the pain. I never really bled alot, just leaked poo mixed with a little blood.
I decided that I didn't want another BM for a while so I cut out solids and went back to a liquid diet for a couple of days to promote faster healing. Really wasn't feasible for me, got too weak so I started eating small meals. My next BM was in the tub, still loose, still burnt like hell.
I know it sounds gross but I'll take gross over that level of pain any day. Here is what I do for a BM which is helping me alot.
1) Soak in a hot bath to relax the lower region and it kinda relaxes the mind. I feel the mind has alot to do with the constriction down below.
2) Let some water out of tub, just keep it deep enough to keep anus covered while lying on back. Keep your head and shoulders up higher due to whats gonna happen next.
3) Have a cold wash rag & bowl of cold ice water next to tub.
4) Have your BM (I normally urinate about the same time), start draining the tub and put the cold wash rag on the anus. Keep it cold by dipping in ice water periodically.
5) When you feel a bit better, do a quick shower to clean the waste off of you and clean the tub. Keep using the cold wash rag if needed.
6) Run another hot bath and soak a while longer to calm the muscles down in the rectum. Keep going back to the cold wash rag as needed.
So far, doing the above I can stay off of the pain meds with an occasional Tylenol. It hasn't been 2 weeks yet, but I've been able to manage the pain with the BM.
I'm in my late 20's, fit, super active, constantly smiling and enjoying life with my two beautiful boys and hubby that was until last Friday (14-03-14) when I underwent a hemorrhoidectomy. I honestly cannot cope with this excruciating pain any longer. My pain threshold is high, I can't stand sitting about but let me tell you, this has knocked me for six. I can manage with the pain between BM's and am doing so with no pain relief (perhaps a couple of ibuprofen) but wow, when that instant pressure comes on i'm straight for the cocodamol, running the bath and getting the gel ready. The pain is like nothing i've felt before (i've had two babies, one natural with no pain relief and one c section!) I am literally screaming out in agony. I'm surprised my neighbours haven't called the police in concern for what the hell is going on!!! The pain I then suffer afterwards for approx 4 hours in unreal. Tonight my husband wanted to call an ambulance as I was literally hysterical. I can't go on like this, I'm scaring myself with the level of panic and sheer despair that i'm feeling. So far this forum has helped me to see that there's light at the end of the tunnel but when I read that people are still experiencing pain 6-18 months later it sends me into a blind panic.
As others have explained, definite lack of info. My surgeon was realistic and said 3-4 weeks recovery but no mention of the side effects (leakage) or anything else. I just thought a week of stinging and soreness, NOTHING ON THIS SCALE
To anyone considering this surgery, I wish I had seen this forum first. People say that people only discuss the negative experiences but read and digest the experiences carefully. I am no shrinking violet but this experience is literally destroying me and that's on day 4!I feel that nobody understands as it's described as a simple op and done on day surgery. I just wish I knew when this hell would be over, that or transport myself back in time!
It looks like the 7-10 days my doctor told me will be accurate--at least (and if you can afford to take the 2 weeks off work, I'd probably suggest it). I did go to work (teacher) for a few hours today and then home to sleep. Walking is annoying and certainly the pain is always there still, but it's really nothing compared to what I expected.
Day 1 pain for me was a 5/6, day 2 was a 3, today (day 3) probably a 3--but it comes and goes.
I think some of the posts on this site are perhaps "premature" in their worries about pain. Everyone is different and everyone's body responds differently to surgery/pain, so I don't think there can be a "predictor" of what you will go through. You might want to go easy and only do a small surgery--one hemorrhoid--first through. See how it goes. But it seems to me that the comments on this site might be the "worst"--my gastro never said anything like these posts (duh), and told me about one man my age who'd lived with them for 20 years who just couldn't believe what it was like to have an easy-to-cl (...)
The BM come quickly and... Pain free! Sensing that was strange, I looked into the bowl immediately and saw only red. I quickly moved to the tub and felt the need to release again. The entire bath turned red instantly. I was laying in the tub, soaking in water, my own blood and feces, and some Epsom salt.
By the time I was admitted and in a room in the ER, I could barely maintain consciousness and, in fact, passed out at least twice, once almost landing with my head on the toilet. The doctors moved me to the ER immediately. After the now familiar burning sensation from the IV, the next thing I remember is waking up in a shared hospital room with an older gentleman. It wasn't difficult to fall asleep again.
When the sun woke me up in the morning, I need some pain medication. The nurse was having trouble understanding that I can't take NSAIDs, which is why I was on Oxycodone the week before. It took hours to get the doctor to order more. Until the early afternoon, all I could do was writhe in agony. These few hours were some of the most excruciatingly painful in my life. Two of the trio of doctors who worked on me showed up at some point. They told me they'd stitched things back up and that I was given two units of blood in the OR and would probably need more.
Throughout the day, I finally got some pain killers and some reasonable food to eat. I even had a BM: soft, wet, dark, and a lot less painful than what I experienced the week before. It felt like the sutures were done better this time around. I also got another unit of blood. The pain killers and my exhaustion meant I could sleep that night and I did, waking up a couple of times to try for #1.
The doctors stopped by the next morning and told me I look a lot better. I replied, “Yeah, I thought I was going to die!†His expression unchanged, one of them paused and replied, “ You lost more than 40% of your blood.†It appears I was on the verge of death upon admission. The doctors kept me there that day and ordered another unit of blood.
I was released the next day and, aside from a couple of small complications, my recovery this time around is going much better than the first week. I do have a small fissure and more hemorrhoids to remove, however. I'm not sure if I'll tackle those the same way. Anyway, I'm happy to be alive, pain and all!
Good luck, everybody.
The first 72 hrs was more difficult than the 30 months of deployments total. When deployed I knew who the enemy was but in this case the enemy was me or my butt. The post surgery pain was extremely excruciating. In between the pain, the spasms, being backed up for four days, the ER visit, laying on the
on the tile bathroom floor for hours and scaring the hell out of the Chick-fil-a customer by screaming Oh My GOD, Oh My GOD in the bathroom. This was the toughest thing I have ever endured. My antidote was taking three Colass in the a.m. and p.m
. and drinking about 90-100 oz of water daily. Accom
I recovered fast and was released to go back to work after 6 weeks. I could have stayed out longer if I thought I needed too because the surgeon asked if I thought I needed more time off and I said no. I was still having a little pain with a bm but that was it. I went back to work and did good for about two weeks. One night we had a lift assist tool go down and I had to lift heavy items for about three hours. The next morning I was in so much pain I could barely get out of bed and I was having very strong spasms. I went back to the surgeon, he did a rectal exam and said that I had tightened up and had become restricted. He took me out of work and gave me stretches to do at home and he put me on Valium, Flexeril, and Hydrocodon. I went for a follow up and he did another rectal exam and said that there was no change and that he wanted me to continue the stretches and he upped the Valium to three times a day and the Hydrocodon to four time a day. I went back two weeks later and he said that there was no change and if he went back in with surgery it could make it worst. He said that there was nothing he could do for me but to set me up with a physical therapist and send me to pain management.
For the therapy it was pelvic floor therapy and I went one day a week for the next 24 weeks and it did not help at all. The pain management doctor changes my meds to Morphine three times a day, Flexeril three times a day and Hydrocodon four times a day. I have had 6 nerve blocks (5 Caudal and 1 Pudendal). They helped a little but did not last. Plus, now I have severe tail bone pain (caused from the nerve blocks) that keeps me from wearing any pants that has a hard seam because I can't stand for the area to be touched. The pain even travels into my penis and causes me to walk kinda bowlegged to keep from anything touching. I cannot sit straight in a chair, I lean to one side or the other. When I have a bm I have to lay down for a few hours because of the pain. I can't drive because I cannot sit straight in the sit plus with the meds I don't think it would be safe. The doctors have me on restrictions of, patient cannot sit for more than 10 minutes, cannot stand for more than 10 minutes, he cannot walk more than 50 yards with out having severe spasms and cannot lift more than 10 pounds. These restrictions plus the meds have kept me out of work for a year and a half. The next step is a Spinal Cord Stimulator implant, we are just waiting on the insurance to approve it. Hopefully if it gives me pain relief so I can come off the meds then I can go back to work.
I have read a lot of blogs since this has happened to me and I know that I am not a lone, because I have found others that are having problems like mine many months or years after this simple surgery. I never really thought of how much pressure is put on the rectum just doing light daily choirs. I can now cause spasms from just getting a gallon of milk from the fridge. I wish I had never had the surgery. I hope by sharing this it may help someone else from going through what I am.
I have not had my first BM yet, but I was told the most important thing is to (eat plenty of fruit and vegetables) for fiber and use stool softeners to keep the BM soft. (Miralax, Benefiber…if those are not enough by third day, take milk of magnesia till you have a BM). If you do not have a significant BM your sphincter can shrink and you will need a second surgery to open back up, so they want you to have a BM at least ever two days.
I cannot believe having no pain, especially after reading all the comments on the internet. I think it is due to a good surgeon Dr. Odom and Exparel (a new product that has been out only a year).
I also use a foam donut to sit on, I bought from Wal-Mart for $12.00 that I use to sit on in my wooden rocking chair that really works. I feel nothing when sitting, but when I stand I feel a little bit of pressure and little soreness for a few minutes.
It will be interesting to see how I feel after the eparel wears off, but up till now NO PAIN, and I am sensitive to pain.
But after doing sex I have pain in my panis for whole day .but next day I have no sex,no pain.
The issue is that I still have small external hemorrhoids and believe the internal are returning as well. This morning I saw that I started bleeding for the first time in a year. I struggle with cleanliness. I usually take my morning shower after.
Considering the complex surgery I had, I almost half expected they might return. I am waiting to see if the bleeding happens again before making a consultation.
The one thing I can recommend to anyone having the surgery, is to do the warm epsom salt baths. It is very relaxing and helps with the pain. I guess I was one who was blessed with minimal pain.
I have no problem if I need to have it redone as I believe it would be less invasive with the smaller external and internal issues.
Every person is different. Most that have no issues following surgery do not find it necessary to post. So, despite the number of failures and extreme pain, remember there are just as many with minimal pain and success.
I had IRC twice which left me with the large externals. Second doctor tried banding 7 times. Nothing else worked until I had the surgery.
This is by far the most pain I've ever been in. After surgery, even with narcotics I was in excruciating pain.
I was in a day surgery ward - 5 hours in hospital, 2.5 of those in surgery.
I went with a high fiber, high liquid diet from the get-go, plus colace.
The first few days it was nearly impossible to even pee. I really needed my husband's physical and emotional support to do so. It is nearly impossible to relax enough to pee.
Warm sitz baths and ice are key. Everything is excruciating. Rest. Sleep. Eat. Drink. Toilet. That's all you should plan on doing. Please have someone help you if at all possible. I had help for a couple days, but I really needed more.
I can not underestimate how difficult toileting is for the first few weeks. Having a BM is like the final push of childbirth, and for me this was many, many times a day in the beginning - like eleven. Over a month later it's down to about six. For the first few week I needed something to hold onto as well. First my husband, then large jugs of water with top handles. After four weeks I could lose the hand holds.
I used a plastic sitz bath that sits on top of the toilet. The warm water really help dilate and relax the spincter. But the spincter will spasm. It hurts like hell. Also, the sutures ooze a bit, and the acid from the BM stings like pouring lemon juice on an open wound. The BM does rip you open.
My case involved internal and external hemmorhoids. They were all very large and the external ones were painful and debilitating. My problem started, like many other posters, with childbirth. Add a stressful job plus taking care of my own children with basically no time off ever...
My surgeon was upfront with me that this surgery has the most painful recovery of any surgery and that I would be suffering for weeks to months.
The upside that I am hoping for is to be rid of the problem foever.
At this point I am over fours weeks post-op. I still cannot go to work. My doctor says I need to rest. I am to avoid sitting and standing and lifting. I tire easily and am still napping.
I still have some oozing from wounds. I stopped bleeding after the first couple of weeks. I keep a log of everything I eat and drink and what I do. I also document every BM and analyze shape, texture and amount to adjust my diet.
What you should have on hand:
- sitz bath
- cup to add hot water to it
- soft ice pack
- Aquaphor (to protect against what can basically become a diaper rash for moisture on the skin around the anus
- mini spray bottle to help clean area
- small gauze pads
- non-stick first-aid pads
- soft clths to wrap ice-pack
- hair dryer (to dry region w/o touching)
- shower
- lots of towels
- fruits & vegetables
- green salads
- grain salads (go easy on gluten)
- fruit & veggie smoothies
- herbal tea
- go easy on dairy & protein - fish is better than red meats
- someone to lean on
- a place to recline
Do not expect to have time for anything but self-care the first couple if weeks. I know it cannot always be avoiding - I had to get work done from home, but self-care will really take up your whole day.
Now, four weeks iut, I am sometimes functional after a BM, sometimes not. I have windows of time during the day when I can do a little. More than short drives does set me back, though. And I really have to watch my diet. It's harder when having to manage other things.
If you have young children, and there's any way you can have them stay somewhere else for a week or two - do it!
Good luck!
I forgot to list the fresh vegetable soups. Those are a big help, too.
I followed up with the surgeon yesterday morning, who said it was healing nicely and it was important that I keep the area dry. I got the okay to go back to work on July 27th. Last night I was trying to give my toddler a bath in an attempt to help hubby. I felt a burning in my anus when i bent over to wash him off in the shower. I called hubby to finish up and sat on the toilet there was fresh blood and having had my daughter take a photo of the area the wound looks opened. I am now wondering if i pulled on the area as I don't remember having such an open wound the first time I had the surgery. Now I am here tossing around the idea if I should go back to the E.R or should i just continue watching the area. I am still in pain and cannot fully sit on my behind. I will appreciate any feedback
1. Make sure your doctor is a board certified COLORECTAL SURGEON!! Not just a general surgeon. AND make sure that surgeon has years of experience doing this procedure.
2. Get your constipation, bowel problems under control BEFORE HAVING YOUR SURGERY!! Otherwise, you just run the risk of developing hemorrhoids again in the future and your recovery will be that much harder. You will most likely develop problems like anal fissures if you don't get your constipation/problems going to the bathroom.
3. If you are a gay man and you have receptive anal sex, you may NEVER be able to participate in that activity again, so think twice before having this surgery.
I had my hemmorhoidectomy done on Thursday and today is Monday. It means I had it 4 days ago.I had 3rd degree of mised hemorrhoid esternal and internal. I must say that I don't have much pain like the others prescribed here. After one day (friday) of my operation I didn't felt any pain but I had problem to pee.. So they had to do the catheter but it was not painful at all only a bit discomfort (I'm a woman). Maye it is different in a man. On my second day I felt the burning on my anus. That kind of pain is almost the same pain that i had before my operation. Same day I had my BM and it went flawless. To be honest I was first very scared to have BM but it was only a little bit pain because on my first day I eat only a banana; yogurt; cerelac (baby food) all day and lots of water (3 liters). A tip when you have your BM you should SQUAT. Watch in youtube. It would make your world a difference; specially to those who had their hemmorhoidectomy operation. I only make BM if I have the feeling that is coming out and don't stay long; if it stop coming out; than stand up; you can still go back if you want ;just don't poop too long. After BM I make a hot seat and it helps with my burning in my anus. Actually; I make a seat bath as much as possible through my days; it can be 6-8 times a day.
Just remember after your operation to drink lot lot of water; eat lots of fiber and if possible consume only fruit; vegetable or oats and cerelac. Squat if you have your BM and don't stay too long.
I think the operation is different in everyone with the pain But suddenly mostly have suffering much. I would do it again because I suffered much with my hemorrhoid before. I'm not really hill yet but I would get better. I would advice you to make the operation if you tried everything with the non success treatments. I know I did not have much pain; but you have to imagine that you would only suffer for 2-3 weeks and your problem is solve instead suffering for a long period of time and it could only get worse if you don't change your life style. I suffered hemorrhoid for 9 years since I give birth to my daughter. I this 9 years I could not walk;jog; lift; or stand too long. I needed everyday to drink medicine so that I could get through my day and when I forgot to intake my medicine the nest day I would suffer. Specially if I went to the grocery or to pick up my daughter to school then I must to find a bathroom to put my hemorrhoid in position back since it goes out to my anus. (sorry I know its grooss) also after I have my BM I needed to push back my hemorrhoid and sometimes it bleed and burn so much; that is why I am happy now where I belong.
I wish all of you good luck heads up. If we can do it than so are you. take it day by day and it can only get better and better. :-) God bless you
1. It wasn't as painful as I thought. I didn't take any of my pain meds because the pain has been very mild and pain meds cause constipation. I took a couple of Tylenols last night to be safe but that's it. I guess it all depends on how many hemorrhoids you get removed because the more scrapping and cutting, the more pain and longer recovery.
2. I was urinating like a horse after the operation, like ever 20 minutes even without drinking liquids.
3. I had 3 bowel movements after the operation and five yesterday and two today. They will come in attack mode so be close to a restroom as you never know when the urge comes. They have been partial as many experienced here.
4. Yes there's discharge and some bleeding every time I have had a bowel movement so I go to the shower and clean the area each time. But the bleeding is less than what I was experiencing over the last two years before the surgery.
5. I take one glass of Miralax a day to soften the stool and will add Benafiber today.
6. I walked to the pharmacy and grocery store right after surgery and the next morning. Walking actually helps.
7. Again it has only been two days so I may have issues over the next few weeks and I don't expect the bleeding to completely stop for 8-10 weeks as my Dr., suggested.
P.S. I also started driving 5 days after surgery and hoping to return to work next week, given I continue to heal as I am :)
P.S. I also started driving 5 days after surgery and hoping to return to work next week, given I continue to heal as I am :)
Any thoughts on how long till I can do a pain free poo
Debbie
Any thoughts on how long till I can do a pain free poo
Debbie
However if you can get over the fact you're wearing a diaper, and nothing else has worked, you may want to try it.
On a good note I do feel better now, The last couple of weeks before I went in I had been feeling weak, could barely walk out to get the mail. Turns out since mine had been bleeding, a lot, I had lost over 2 pints of blood, While in for the hospital I recieved a total of 4 units of blood, about 4-6 units of Iron and a lot of IV Drips. The only reason I even went to the Hospital is because on the 13th, my boss dropped by before heading to our other store and told me how pale I looked, which I wasn't even aware of, as we walked up to her store she told me constantly to go to the hospital, glad she did, as If I had been any lower in blood I'd have been a corpse. I know hear our accounts may have many thinking, "Maybe I'll wait", Don't. Waiting nearly killed me, yes the recovery isn't pleasant, but its certainly alot better than the constant pain and possibly death. Go see a Dr.
Hope these days that have passed are better for you. I'm now 25 days post op and the pain is just now starting to subside after I have BMs (still a little irritation but no Motrin or Tylenol) and the site is feeling more smooth. I've been advised to continue sitz baths (I've been adding Epsom salt) 4 times a day going on week 4 until my next follow up appointment and ensure I'm keeping up on my water intake and to include more walking. I've been mixing the miralax w/ honey and green tea in the mornings. My stools have been the same as you describe. Just speaking from my experience I think it's just the healing process opening and closing the wound from BMs will just a take a while to heal. Is the on call nurse available in the doctors absence? Perhaps he/she may be able to help? We will get thru this. Hang in there.
I have not read anyone else saying that their Doctor administered an injection that managed pain for up to three days. Both hospitals that I went to told me that they would numb me up and that it would last up to three days - hopefully to get you past the first bowel moment. I had surgery and then went home a few hours later with no feeling in my bottom. I woke up frequently that night, but not from pain. Just recovering from the surgery general I believe. The next day I had discomfort. I couldn't really get comfortable, so I paced around the entire day with occasional sitz baths for soothing. I didn't take any pain meds. The next morning I could tell the numbing shot was wearing off and that was the first time I took any meds. Although I was sent home with pain drugs - I was also told that they would most likely make me nauseous and cause constipation. I took 3 Ibuprofen (600mg) and I did get relief. I alternated this dose of Ibuprofen with 2 extra strength Tylenol for the next few days without ever having to take a prescription pain pill. I took miralax every day to keep my stools soft and raised my feet onto a stool when I needed to poop. I cannot stress enough how important it is to stay relaxed when having a bowel movement. You just have to relax and let it come and be ready to soak in the bath after to cleanse and soothe. I sat in the bath multiple times a day and got relief from that. I will say that when I HAD my hemorrhoids the sitz bath did NOT help, so I was so happy that it did help post surgery. I am typing this on Wednesday and I had the surgery late afternoon the previous Thursday. Today, I have only taken three ibuprofen the entire day and will be going to bed soon without any additional medication. I will say that I am taking it very easy and did not schedule this until my husband was able to take two entire weeks off to be with me to help with our three teenagers. I really feel that a key to recovery is to rest, hydrate and be prepared so that you are not caught in the throws of pain and panic. I was PETRIFIED of this surgery because of all the hellish things I read, and I want others reading this to know, that it isn't always the worst case scenario. Perhaps the people that don't have terrible issues don't take the time to tell others that it wasn't too bad. Don't get me wrong - it hurts a lot, but I didn't experience crying or screaming or gushing of blood or severe swelling or anything like that. I am very bruised and have all sorts of stitches, but it seems to be healing really well. I am 46 year old woman. I am so glad that I did not chicken out and not have the surgery, I just couldn't imagine my entire life with these hemorrhoids and knew that the older I got - the harder it would be to have the procedure done.
I had my operation on 26th of August and i was physically feeling great after and surgeon also told me that apart from removing skin tag he has also removed internal hemorrhoid - great! I was given two types painkillers (ibuprofen and dihydrocodeine), antibiotics (metronidazole) and movicol liquid to drink twice a day. When i got home i was quite afraid to drink movicol at that stage as i didn't want to go tho the bathroom just yet. That was the biggest mistake. Once you leave hospital you need to start drinking as anesthesia makes feces hard. I had first BM around 4am the following morning and i was in extreme pain. I took hot shower to sooth the area and went for the strong painkillers.
1st week - I kept having painful BM twice a day that week but the shower and painkillers kept the pain in bay. During the first week somehow i managed to catch flu.
2nd week - I noticed that the incisions came apart, were sore and still i was getting a bit of blood in my discharge. I went to my GP same day. After examination he said, which was quite alarming, he didn't know what the surgeon has done. There were no stitches and instead of removing the skin tag the surgeon removed just half of it and managed to create another one! The GP sent me back home with another dose of antibiotics. Also I stopped taking painkillers at the beginning of that week.
3rd week - I, at last, felt like i started to heal! The discharge almost stopped, the BM were just a bit uncomfortable and the pain would disappear just after BM, i had more energy and gone back to work.
4th week - I had some blood during BM and the pain came back to the point where i had to take strong painkillers to control it. I thought i would be just one day but i was feeling pain the following day as well. I called my GP and i went to see him same morning.He again said that he wasn't sure what the surgeon has done, there was still discharge, the external skin tags were swollen as well as internal wall where the incision were. As i have hospital appointment in to weeks time my GP said that the appointment cannot be moved and he can't send me to hospital as this is not an emergency. I was sent away with two creams. One, which is Bactroban - an antibiotic, has been quite helpful and i need to apply on the skin tags and the area three times a day. Other cream that i was given is called Germoloids which is an ointment for piles. This i was told to apply twice a day till my hospital appointment. I used that cream twice and in both cases i experience a lot of pain so I stopped using that.
My case might me a bit extreme compared to others and somehow i wish i didn't go with it.
Worse then childbirth
Day 1 through Day 4 was pretty miserable. Not just the discomfort although that was bad enough but the real issue was constipation. My surgeon only had me empty my lower GI and didn't have me start laxative or stool softeners pre-surgery. As a result, my first movement was large, hard and very painful. Afterward I felt like I had just undergone a second hemorrhoidectomy. The pain was severe and like others I didn't get much relief from Percocet alone. Percocet really only made me sleepy however Percocet with Motrin was the perfect cocktail. Once you get past that first movement it was fairly manageable. The pain is very real and sustained for the first 5 days but after that it decreased rather quickly. The pain was limited to bowel movements which I did on the toilet (not in a sitz bath as others have suggested). Each movement got a little better. I'm basically pain free today and I get around just fine. I cannot sit for extended periods of time without aggravating the area however and when I do and the swelling follows everything become more challenging.
Advice:
- Start the stool softeners at least 48 hours in advance of your surgery.
- Empty your upper and lower GI prior to surgery so your system has a fresh start before your first bowel movement.
- Do not allow your pain medication window to expire during the first week. If you go too long before doses and the pain becomes aggravated it will take an extended period to offset the pain.
- Sitz baths after every BM is a must for both keeping the wound clean and to promote healing.
- Adopt the high fiber diet meaning 150% of the daily recommended amount (Metamucil 2x/day, Stool softener 2x/day, at least a liter and a half of water per day, drink a glass of water first thing in the morning even before you brush your teeth and wait 45 minutes before eating.)
- Don't stay in bed. Move around within reason to keep your metabolism moving.
The pain was very bad in the early going but I would do this surgery again ten times over if it meant never having to deal with the hemorrhoids again. My life is greatly improved. What used to be an ordeal in the bathroom is now a 5-7 minute experience and I'm done.
Good luck to you all.
It seems that about 15% of people handle this well with only short term pain. Another 15% have horror stories as mentioned above. The remaining 70% follow a similar journey as I have. The above stories of strong pain and discomfort are similar to mine. I see the post op as four stages:
Days 1-5: Awful pain especially with BMs
Days 6-10: becoming tolerable with some improvement
Days 11-14: adjusting and starting to see light at end of tunnel
Day 15+: actual healing and recuperation
My recommendations, similar to what you read above as as follows:
1. High fiber, stool softeners, laxatives, and lots of water especially in first few days
2. Hot baths, as hot as you can handle, are critical
3. Avoid opioid painkillers due to constipation. Cycle ibuprofen and Tylenol as tolerable
4. Keep area clean, use lots of gauze and creams
5. Exercise. This may seem counterintuitive but slow running took the pain away
6. Have a drink if needed!
I would avoid this procedure unless there is no other option. You will get through it but it’s a rough ride. I’ve had kidney stone surgeries, pilonidal surgeries, and others. This post op is BY FAR the worst.
I have been in pain the last 6 days with a Hemorrhoid, a very, very painful bout. Went to ER about 4 days ago and they said it looks OK and to contact a surgeon, may need it removed. I've been reading a lot about this and just happened to come across this site and the various contribution posts you all have provided over the last 8 years. And from my reading of all your posts I will do all I can to NOT have any surgery for this. The posts on the major after-surgery pain and post-op recovery time has me already making changes to my diet. Believe me, I will do all I can to never have to do this.
Thank you, each and every one of you, for your advise, options, opinions, and information. I hope and pray that you all have not gotten through your pain and are now better.
I had a colon resection years ago, my very first nightmare of a surgery and recovery. I thought I would die from the pain and at times, wished I was dead. So reading all the bm pain everyone dealt with takes me back to that surgery. I must of had 40 bm in one day. It was like someone poured acid on open wounds. I was told to use the sitz bath which did give comfort. Most of the time I just pooped in that. I don't want to relive that and that is what this sounds like. I know that hell!!! So I am scared to death knowing what I know. My husbands tells me to do it, get it over with... Easier said than done, especially if you're not one suffering.
I thank everyone for taking the time to share your story. It is a great help indeed. You are the true warriors!!!
I had my conventional hemorrhoidectomy on 17/11/2018 removed 3 anal cushions ( 3 internal hemorrhoids grade 3 )
I did go home after the surgery
The first day home when the anesthetic did go away , I had intense pain all day nothing helped I took opioids but the first 4 hrs were crazy
Intense pain all day
Second day It was better all the time I was taking opioids and paracetamol
3rd day I woke up the bed was all blood
I was bleeding everywhere
Did go to emergency immediately and ended up in operation room one more time
This time for two hours they I was bleeding alot from everywhere
Woke up after operation high on morphine and anesthetics didnt feel anything and stayed on hospital for two nights
So now im 5 days post surgery and didnt have any bowel movements
Did go home on 6th day
They gave me enema to have a bowel movement which I had
The worst pain in my life was at that first bowel movement
Second bowe movement was also intense in pain i was screaming in the WC
It was like that till my seventh bowel movement improved with pain which was 10th day after second surgery
Pain lasts 4hrs after bowel movement
With discomfort and rectal tenesmus ( feeling always I need to poo even when I have had bowel movement ) feeling this all day worst feeling ever .
Today its my 13th day post surgery I take everyday lazatives and fiber so I womt scream that much in WC
Still in pain and discomfort all day have the feeling I want to poo especially when Im walking
So expect to get 3-4 weeks off nothing less than that .
Do I recommend the surgery ?
For me never I had 3rd degree Internal hemorrhoids which I could manage .. with diet and some activity , I regretted that I did the surgery .
For 4th degree and unmanagable hemorrhoids which always bleed or prolapse I would recommend it but the first 3 weeks you’ll feel uncomfortable all time and you’ll be in pain
For me it was the worst experience in my life
I donr know how much more time I need to get back to my normal life and normal activity I cant do anything
I Did not bleed right after surgery though the pain was intense for one week. It got better and I went on to a normal diet and even started exercising. I have coffee as well and though I am not severely constipated I do strain. I have not had a BM without a bit of straining even though I take meds as prescribed.
has anyone else had bleeding clots with BM?
I had excissional hemorhoidectomy 1 week ago, i was suffering with hemorhoids for 15 years. due to this problem i always used to get sick very often bcoz of losing blood in stools, and felt nervous. i can't stand long time . it was paining like anything. i went so many hospitals,took so many medicines nothing got worked out. i had internal,external,prolapsed,bleeding,hemos grade 4 hemos with skin tag. in 2014 i had 2 rubberband procedures for them which was worked better but though i lost much blood from hemos. my son was born it was natural delivery that time the external ones became worse. so i scared like anything to go with hemorhoid surgery.but in 2019 april 11 i had the surgery the doctor said that u gonna hate me after the procedure, even though i stepped forward so they gave me pain medication through IV. in fraction of seconds i went complete in sleep. so my procedure it took for 20 mins, max i was in hospital 4 hours it was an outpatient surgery. thatday i couldn't seen any pain until the next day mrng.i was taking pain medicines time to time. also laxatives fibre supplement( miralax,milk of magnesia, citrucel) the first BM was so painful was screaming like anything. i was taking so much water and at the same time pain medicines laxatives, for first 3 days it was horrible for me could not pass gas, could not go BM, couldnot pee. so i called the doctor for pain they suggested me take Lidocaine numbing ointment. which is not worked for me. whenever i pee or feeling to go BM i use sitzbath and hot bath.these are the only two thing which can protect u in this surgery pain medicines too but will get constipation. i took everything like chain . so the 3 rd day i had loose motion that time the difficuty passage of stools not bothered that much.i couldnot drop anything ,i was taking everything without lefting anything .the 4 th day i can able to manage pain but first time the sharp pain immediately used sitzbath. i didn't strained for the intolerate pain.whenever i feel BM i used hot water shower after that wiped with baby wipes. 5 th day i felt comfortable,6 th day i was able to walk, and the 7 th day i became completely normal person, today 8 th day i am back to normal work actitivies ,i went to walking for some time which is very happiest day for me no pain at all while BM too. i started sitting on pillow also. i used to eat roties vegetable curries (only fiber food) i didn't touched any rice or outside foods ,if u want u can drink soups. but onething i can say don't scare and don't step back for your problems, everyone's case is different. if u want to permanent relief u have to go through temperory discomfort. if u scare for the procedures u hv to go through lifelong problem.so one thing i can say everyones body is different,case is different. i thought that this is the scariest procedure. but NO. if u want happy life then u have to go through worst part . honestly for me the worst days are just 3 to 4 days. i suffered 15 years like anything. everyone said horror stories and i read also about this. but that is not 100% true (again case to case). please don't scare .your scary thoughts only destroy u, not ur health. if anyone gone through my story please step forward only few days 3 to 4 crucial days other than that happy life..
This isn’t some random training... I just got the inside scoop that they will be exposing how you can profit from a pretty much “hidden†$355 million dollar a day industry that’s expected to TRIPLE within the next 5 years according to Forbes.
So whether you have your own business, want to start one or just want to create more income for you and your family – you’re not going to want to miss this training right from the comfort of your own home...
Even better... these guys are all about making an impact on the world and they want to help US do the same thing while WE get paid for it…
Tony hasn’t done a training like this in over 10 years – so no way I’m missing it.
Use this special link I got and go register now... the spots and chat are limited so make sure to show up early so we can ask them questions at the end...
https://dgachieve.com/joining?source=wowspeciallink&a=2543
Isn’t it most all of our dreams to make an impact, leave a legacy and generate the type of income that allows us to have control of our time and decisions?
That’s exactly what Dean & Tony have mastered like no other and for the first time ever on a training, they’re going to show us how to accomplish all of those same goals.
There may never be another chance again in history to see these guys, sharing the secrets they have learned over a combined 62 years of business and impact...
If you are ready for your next level then you won't want to miss this. Because if not them now... Then who and when?
Use this special link I got and go register now... The spots and chat are limited so make sure to show up early so we can ask Dean and Tony questions at the end...
https://dgachieve.com/joining?source=wowspeciallink&a=2543
Plus they did an all new “quick pre-event†training you’ll get instant access to once you reserve your spot.
See you there
Those words re scary but as u said is my life. The torment of bleeding , not eating normal food or even removing ur boxes where people re is heartbreaking. Will be going for the op in china . God is with me
It was tough not eating regular food for three week; but I did it to assure all my BM were soft and to eliminate any pain. Yes, there was some minor pain my first week but I got use to it. I followed every post-op my Doctor instructed me to do and she was spot-on on how it was going to be. I did not do a sitz bath at all. I did however; take very warm almost hot showers hot enough to tolerate the heat while rinsing. It did ease the pain for sure. I did take my pain medicine up until I could tolerate the pain on my own, just due to the fact that I don’t like to pump medication into my body if I don’t need to. I drank plenty of water and protein shakes which helped 1) satisfied my hunger and 2) kept my daily nutrition going. Also, don’t forget to take a laxative such as Miralax or Metamucil. I drank my Metamucil three times a day and it helped with my BM. Also, during my BM’s, I used an aloe type baby wipe then immediately took a warm shower.
Sitting down was a nuisance for about 2.5 weeks due to the stitches so I stood or sat on one side of my buttocks. Sleeping was an issue for me too, while I am a back sleeper, it was quite painful to lay on my back bit sleeping on my side did the trick. So, on my third week, two stitches busted and I ended up in the ER. I bled quite a bit, but the ER staff got in under control and I was on my way home after almost five hours in the ER. As of today, 07 November 2019, I do have a skin tag but that was explained to me during my consultation with my surgeon. She did say it was normal in some cases and will eventually shrink with time - I trust her. I am fortunate enough the Navy gave me 30 days of convalescence leave to recover, I know most of you cannot get that type of time off, but I’m sure if you asked your Doctor they would provide you that time.
I decided to post my experience with you all because I see there are a few of you with second thoughts, but believe me, I’ve had hemorrhoids for nearly 15 years and it was just getting worse so I decided to take the chance and get it done. I’m recovering well but not enough to continue my normal lifestyle of hiking, CrossFit, spear fishing, and shooting my bow - can’t wait to get back to 100% and continue on with life. To sum it all up and provide you with my takeaway, just follow your Doctors orders exactly how he or she told you, take it easy, don’t be stubborn and think you are invisible and re-injure your rectum. If there’s one thing I would recommend, it would be to take your pain meds as prescribed for the pain and keep your bottom clean as much as you can. I cleaned with Dial soap because it’s an anti bacterial soap and it worked for me, but use what works for you of course. Hope this helps and don’t be afraid, you’I’ll be alright.
Thank you
Had my surgery on Jan 12, 2020.
It is now Jan 31.
I had one very large (according to the surgeons) hemorrhoid, a smaller one (which I wasnt aware of), and a fissure, which they said was causing me the majority of the pain when passing stool.
The large hemorrhoid wasnt exactly external, but it would always poke out when passing stool.
Each time I passed stool, it felt like my insides were being ripped apart, and I bled every single time.
I endured this for over 10 years.
It made me fearful to use the bathroom, especially outside the comforts of my home, and so affected my every day venture outside of my house.
Every trip outside had to be planned and prepared for careful.
I had seen 2 doctors before my current one, and they all recommended I take more fibre.
But I did not have a constipation problem.
I had a phobia of having to use the bathroom outside my home, which made my hemorrhoids worse, because I would force myself to sit on the toilet till I felt "empty".
So even though I did not suffer hard stool, I was still forcing myself to sit on the toilet for over an hour, to make sure I passed out enough stool to feel like I could survive a day outside.
So that is my hemorrhoid history.
I eventually found a doctor on October 2019, who said that surgery would solve my pain and bleeding problems.
The large hemorrhoid was cut out, and the smaller one was bound, which he said would have fallen off by now, and an incision was made beside the fissure, as a new cut would help a stubborn cut to heal. I dont understand the logic, but ok.
I was made to stay a night at the hospital after the surgery, which was a good idea, as I had so much difficulty passing urine that night, and had to have a catheter inserted.
Catheters are awful.
The pain was terrible, but I found out that it was due to the packing that was inserted and left in overnight.
I had minimal bleeding that night, but a lot of pain.
The day I left the hospital, when the doctor inspected me and removed the packing, that was the worst pain I felt this entire recovery period.
I was able to move around, climb stairs (room is on 2nd floor), and was able to eat regular food right away.
Did not pass stool till the 2nd day at home, and can I tell you, THERE WAS NO PAIN!!!
THERE WAS NO BLEEDING!!!
Over 10 years of pain and bleeding, and I almost wept when there was none of that!!
I am so so happy that I did it.
There is some pain, especially when I unconsciously clenched for whatever reason.
I felt mainly sore.
I saw in salt water sitz bath after each stool passing, very tiresome, which was a lot, because I was taking extra fibre and stool softeners.
Wore diapers, because I couldnt control down there. Have more control now, but I wouldnt push my luck, if I feel the urge to go, I will run to the bathroom.
There is some oozing, but the diapers takes care of that. I think I can move on to liners now.
I also use witch hazel wipes, and smear the area with vaseline and calmoseptine.
Now, I soak a cotton ball in salt water, and dab the area to make it clean, since I can tolerate touching the area now.
I still have open wounds down there.
I had also read the comments on this site right up to the day of my surgery, and I had scared myself silly, but also took away a lot of advice on what to expect and what to do after.
I feel sorry for everyone that has experienced and is still experiencing pain from this surgery.
But compared to what I endured before, I wish I had done this sooner, but maybe I wouldnt have found the right surgeons.
So do your researches, and good luck!
And know that there is a chance for a smooth recovery.
Had my surgery on Jan 12, 2020.
It is now Jan 31.
PS, I took 2 weeks off from work.
Also, coughing and sneezing sucks.
I was fully anesthetized for the surgery. Im not sure how long it took either.
I was given soft foods after surgery and my 1st day back home, but solids from then on.
I was given 2 weeks of antibiotics, and my pain medicine was baralgim.
I could move around with minimal pain, but sitting and sitting up from a lying position did cause me some pain during the 1st 2 weeks.
More like a soreness.
But Im fine now.
Only sneezing and coughing really hurt, even now.
Had my surgery on Jan 12, 2020.
It is now April 7
About 98% healed.
The incision area is only the tiniest bit sore if I put significant pressure on it.
100% happy that I did this surgery.
Ive long forgotten how painless passing stool should be!
Please how long did you continue taking the stool softeners and fiber supplements (if any) after the surgery? How is passing stool like after you stopped them? I'm 24 days post op and I can tell you i feel no pain at all, only mild discomfort during BM. Though I'm still on the stool softener and fybogel, my stool seems to be irregularly as compared to the early days after the surgery