Gastroesophageal reflux surgery
Definition
Gastroesophageal reflux surgery is typically performed in patients with serious gastroesophageal reflux disease that does not respond to drug therapy. Gastroesophageal reflux is classified as the symptoms produced by the inappropriate movement of stomach contents back up into the esophagus. Nissen fundoplication is the most common surgical approach in the correction of gastroesophageal reflux. The laparoscopic method of Nissen fundoplication is becoming the standard form of surgical correction.
Purpose
Gastroesophageal reflux surgery, including Nissen fundoplication and laparoscopic fundoplication, has two essential purposes: heartburn symptom relief and reduced backflow of stomach contents into the esophagus.
Heartburn symptom relief
Because Nissen fundoplication is considered surgery, it is usually considered as a treatment option only when drug treatment is only partially effective or ineffective. Nissen fundoplication is often used in patients with a particular anatomic abnormality called hiatal hernia that causes significant gastroesophageal reflux. In some cases, Nissen fundoplication is also used when the patient cannot or does not want to take reflux medication. Surgery is also more likely to be considered when it is obvious that the patient will need to take reflux drugs on a permanent basis. Reflux drugs, like virtually all drugs, may produce side effects, especially when taken over a period of years.
One of the biggest problems in diagnosing and controlling gastroesophageal reflux disease is that the severity of disease is not directly related to the presence or intensity of symptoms. There is also no consistent relationship between the severity of disease and the degree of tissue damage in the esophagus. When reflux occurs, stomach acid comes into contact with the cells lining the esophagus. This contact can produce a feeling of burning in the esophagus and is commonly called heartburn. Some of the other symptoms associated with this condition include:
- chest pain
- swallowing problems
- changes in vocal qualities
Reduced reflux
The reduction or elimination of reflux is as important, and sometimes more important, than the elimination of symptoms. This necessity leads to one of the most important points in gastroesophageal reflux disease. Long-term exposure to acid in the esophagus tends to produce changes in the cells of the esophagus. These changes are usually harmful and can result in very serious conditions, such as Barrett's esophagus and cancer of the esophagus. Because of this, all persons with gastroesophageal reflux disease symptoms need to be evaluated with a diagnostic instrument called an endoscope. An endoscope is a long, flexible tube with a camera on the end that is inserted down the throat and passed all the way down to the esophageal/stomach region.
All gastroesophageal reflux surgery, including Nissen fundoplication, attempts to restore the normal function of the lower esophageal sphincter (LES). Malfunction of the LES is the most common cause of gastroesophageal reflux disease. Typically, the LES opens during swallowing but closes quickly thereafter to prevent the reflux of acid back into the esophagus. Some patients have sufficient strength in the sphincter to prevent reflux, but the sphincter opens and closes at the wrong times. However, this is not the case in most individuals with gastroesophageal reflux disease. These individuals usually have insufficient sphincter strength. In a small number of cases, the muscles of the upper esophagus region are too weak and are not appropriately coordinated with the process of swallowing.
The development of heartburn does not necessarily suggest the presence of gastroesophageal reflux disease, which is a more serious condition. Gastroesophageal reflux disease is often defined as the occurrence of heartburn more than twice per week on a long-term basis. Gastroesophageal reflux disease can lead to more serious health consequences if left untreated. The primary symptoms of gastroesophageal reflux disease are chronic heartburn and acid regurgitation, or reflux. It is important to note that not all patients with gastroesophageal reflux disease have heartburn. Gastroesophageal reflux disease is most common in adults, but it can also occur in children.
The precise mechanism that causes gastroesophageal reflux disease is not entirely known. It is known that the presence of a hiatal hernia increases the likelihood that gastroesophageal reflux disease will develop. Other factors that are known to contribute to gastroesophageal reflux disease include:
- smoking
- alcohol ingestion
- obesity
- pregnancy
The following foods and drinks are known to increase the production of stomach acid and the resulting reflux into the esophagus:
- caffeinated drinks
- high-fat foods
- garlic
- onions
- citrus fruits
- chocolate
- fried foods
- foods that contain tomatoes
- foods that contain mint
- spicy foods
Most patients take over-the-counter antacids initially to relieve the symptoms of acid reflux. If antacids do not help, the physician may prescribe drugs called H 2 blockers, which can help those with mild-to-moderate disease. If these drugs are not effective, more powerful acid-inhibiting drugs called proton-pump inhibitors may be prescribed. If these drugs are not effective in controlling gastroesophageal reflux disease, then the patient may require surgery.
Demographics
It has been estimated that heartburn occurs in more than 60% of adults. About 20% of the population take antacids or over-the-counter H 2 blockers at least once per week to relieve heartburn. In addition, about 80% of pregnant women have significant heartburn. Hiatal hernia is believed to develop in more than half of all persons over the age of 50 years. Hiatal hernia is present in about 70% of patients with gastroesophageal reflux disease, but the majority of patients with hiatal hernia do not have symptoms of gastroesophageal reflux disease. In addition, about 7-10% of the population has daily episodes of heartburn. It is these individuals who are likely to be classified as having gastroesophageal reflux disease.
Description
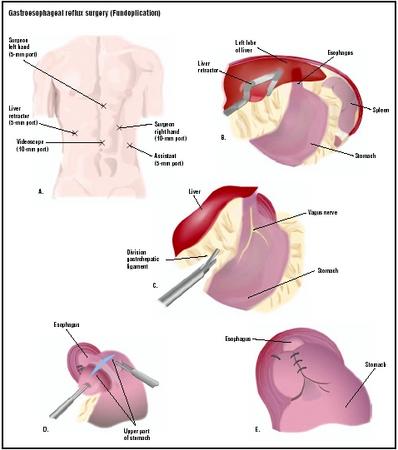
The most common type of gastroesophageal reflux surgery to correct gastroesophageal reflux disease is Nissen fundoplication. Nissen fundoplication is a specific technique that is used to help prevent the reflux of stomach contents back into the esophagus. When Nissen fundoplication is successful, symptoms and further damage to tissue in the esophagus are significantly reduced. Prior to Nissen fundoplication, open surgery was required to gain access to the lower esophageal region. This approach required a large external incision in the abdomen of the patient.
Fundoplication involves wrapping the upper region of the stomach around the lower esophageal sphincter to increase pressure on the LES. This procedure can be understood by visualizing a bun being wrapped around a hot dog. The wrapped portion is then sewn into place so that the lower part of the esophagus passes through a small hole in the stomach muscle. When the surgeon performs the fundoplication wrap, a large rubber dilator is usually placed inside the esophagus to reduce the likelihood of an overly tight wrap. The goal of this approach is to strengthen the sphincter; to repair a hiatal hernia, if present; and to prevent or significantly reduce acid reflux.
Fundoplication was greatly improved with the development of the laparoscope. The laparoscope is a long thin flexible instrument with a camera and tiny surgical tools on the end. Laparoscopic fundoplication (sometimes called "telescopic" or "keyhole" surgery) is performed under general anesthesia and usually includes the following steps:
- Several small incisions are created in the abdomen.
- The laparoscope is passed into the abdomen through one of the incisions. The other incisions are used to admit instruments to manipulate structures within the abdomen.
- The abdomen is inflated with carbon dioxide. The contents of the abdomen can now be viewed on a video monitor that receives its picture from the laparoscopic camera.
- The stomach is freed from its attachment to the spleen.
- An esophageal dilator is passed through the mouth into the esophagus. This dilator keeps the stomach from being wrapped too tightly around the esophagus.
- The portion of the esophagus in the abdomen is freed of its attachments.
- The top portion of the stomach (the fundus) is passed behind the esophagus, wrapped around it 360°, and sutured in place.
- If a hiatal hernia is present, the hiatus (the hole in the diaphragm through which the esophagus passes) is made smaller with one to three sutures so that it fits around the esophagus snugly. The sutures keep the fundoplication from protruding into the chest cavity.
- The laparoscope and instruments are removed and the incisions are closed.
Diagnosis/Preparation
The diagnosis of gastroesophageal reflux disease can be straightforward in cases where the patient has the classic symptoms of regurgitation, heartburn, and/or swallowing difficulties. Gastroesophageal reflux disease can be more difficult to diagnose when these classic symptoms are not present. Some of the less common symptoms associated with reflux disease include asthma, nausea, cough, hoarseness, and chest pain. Such symptoms as severe chest pain and weight loss may be an indication of disease more serious than gastroesophageal reflux disease.
The most accurate test for diagnosing gastroesophageal reflux disease is ambulatory pH monitoring. This is a test of the pH (a measurement of acids and bases) above the lower esophageal sphincter over a 24-hour period. Endoscopies can be used to diagnose such complications of gastroesophageal reflux disease, as esophagitis, Barrett's esophagus, and esophageal cancer, but only about 50% of patients with gastroesophageal reflux disease have changes that are evident using this diagnostic tool. Some physicians prescribe omeprazole, a proton-pump inhibiting drug, to persons suspected of having gastroesophageal reflux disease to see if the person improves over a period of several weeks.
Aftercare
Patients should be able to participate in light physical activity at home in the days following discharge from the hospital . In the days and weeks following surgery, anti-reflux medication should not be necessary. Pain following this surgery is usually mild, but some patients may need pain medication. Some patients are instructed to limit food intake to a liquid diet in the days following surgery. Over a period of days, they are advised to gradually add solid foods to their diet. Patients should ask the surgeon about the post-operative diet. Such normal activities, as lifting, work, driving, showering, and sexual intercourse can usually be resumed within a short period of time. If pain is more than mild and pain medication is not effective, then the surgeon should be consulted in a follow-up appointment.
The patient should call the doctor if any of the following symptoms develop:
- drainage from the incision region
- swallowing difficulties
- persistent cough
- shortness of breath
- chills
- persistent fever
- bleeding
- significant abdominal pain or swelling
- persistent nausea or vomiting
Risks
Risks or complications that have been associated with fundoplication include:
- heartburn recurrence
- swallowing difficulties caused by an overly tight wrap of the stomach on the esophagus
- failure of the wrap to stay in place so that the LES is no longer supported
- normal risks associated with major surgical procedures and the use of general anesthesia
- increased bloating and discomfort due to a decreased ability to expel excess gas
Complications, though rare, can occur during fundoplication. These complications can include injury to such surrounding tissues and organs, as the liver, esophagus, spleen, and stomach. One of the major drawbacks to fundoplication surgery, whether it is open or laparoscopic, is that the procedure is not reversible. In addition, some of the symptoms associated with complications are not always treatable. One study showed that about 10% to 20% of patients who receive fundoplication have a recurrence of gastroesophageal reflux disease symptoms or develop such other problems, as bloating, intestinal gas, vomiting, or swallowing problems following the surgery. In addition, some patients may develop altered bowel habits following the surgery.
Normal results
One research study found that fundoplication is successful in 50% to 90% of cases. This study found that successful surgery typically relieves the symptoms of gastroesophageal reflux disease and esophagus inflammation (esophagitis). The researchers in this study, however, provided no information on the long-term stability of the procedure. Fundoplication does not always eliminate the need for medication to control gastroesophageal reflux disease symptoms. A different study found that 62% of patients who received fundoplication continued to need medication to control reflux symptoms. However, these patients required less medication than before fundoplication.
Two studies demonstrated that laparoscopic fundoplication improved reflux symptoms in 76% and 98% of the treated populations, respectively. In an additional study, researchers evaluated 74 patients with reflux disease who received Nissen fundoplication after failure of medical therapy. The researchers concluded that 93.8% of the patients had complete resolution of symptoms and did not require anti-reflux medications approximately 14 months after fundoplication. Researchers have found that when fundoplication is successful, the resting pressure in the LES increases. This increase reflects a return to more normal LES functioning where the LES keeps stomach acid in the stomach through increased pressure.
Overall, studies have suggested that the vast majority of patients who receive laparoscopic reflux surgery have positive results. These patients are either symptom-free or have significant improvements in reflux symptoms. The laparoscopic approach has a few advantages over other forms of fundoplication. These advantages include:
- decreased postoperative pain
- more rapid return to work
- decreased hospital stay
- better cosmetic results
Morbidity and mortality rates
Mortality is extremely rare during or following fundoplication. Complications and side effects are not common following fundoplication, especially using the laparoscopic approach, and are usually mild. A review of 621 laparoscopic fundoplication procedures performed in Italy found no cases of mortality and complications in 7.3% of cases. The most serious complication was acute dysphagia (difficulty swallowing) that required a re-operation in 10 patients. In general, long-term complications resulting from this procedure are uncommon.
Alternatives
There are several variations of fundoplication that may be performed. In addition, laparoscopic fundoplication may require conversion to an open, or traditional, surgical fundoplication in a small percentage of cases. The most common alternative to fundoplication is simply a continuation of medical therapy. Typically, patients receive medication for a period prior to being evaluated for surgery. A review of nine studies found that omeprazole, a proton-pump inhibitor, was as effective as surgery. This same review, however, found that the other commonly used anti-reflux drugs, histamine H 2 -antagonists, were not as effective as surgery.
Resources
books
Current Medical Diagnosis & Treatment. New York: McGraw-Hill, 2003.
Ferri, Fred F. Ferri's Clinical Advisor. St. Louis, MO: Mosby, 2001.
periodicals
Allgood, P. C., and M. Bachmann. "Medical or Surgical Treatment for Chronic Gastroesophageal Reflux: A Systematic Review of Published Effectiveness." European Journal of Surgery 166 (2000): 9.
Kahrilas, P. J. "Management of GERD: Medical vs. Surgical." Seminars in Gastrointestinal Disease 12 (2001): 3–15.
Scott, M., et al. "Gastroesophageal Reflux Disease: Diagnosis and Management." American Family Physician 59 (March 1, 1999): 1161–1172.
Society of American Gastrointestinal Endoscopic Surgeons. "Guidelines for Surgical Treatment of Gastroesophageal Reflux Disease (GERD)." Surgical Endoscopy 12 (1998): 186–188.
Spechler, S. J., et al. "Long-term Outcome of Medical and Surgical Therapies for Gastroesophageal Reflux Disease: Follow-Up of a Randomized Controlled Trial." Journal of the American Medical Association 285 (May 9, 2001): 2331–2338.
Triadafilopoulos, G., et al. "Radiofrequency Energy Delivery to the Gastroesophageal Junction for the Treatment of GERD." Gastrointestinal Endoscopy 53 (2001): 407–415.
Zaninotto, G., D. Molena, and E. Ancona. "A Prospective Multicenter Study on Laparoscopic Treatment of Gastroesophageal Reflux in Italy." Surgical Endoscopy 14 (2000): 282–288.
other
National Digestive Diseases Information Clearinghouse. Heartburn, Hiatal Hernia, and Gastroesophageal Reflux Disease (GERD). 2003.
Society of American Gastrointestinal Endoscopic Surgeons. Patient Information from Your Surgeon and SAGES. 1997.
Mark Mitchell, M.D., M.P.H., M.B.A.
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Fundoplication, including the laparoscopic approach, is generally performed by a specialist known as a gastroenterologist. A gastroenterologist is a medical doctor (M.D.) who has received additional training in the diseases of the gastrointestinal system. Gastroenterologists who perform laparoscopic fundoplications receive extensive training in general surgery and in the proper techniques involving the use of the laparoscope. If surgery is being considered, it is a good idea to find out how many laparoscopic fundoplications the surgeon performs on a yearly basis. Laparoscopic fundoplications are often performed in the specialized department of a general hospital, but they are also performed in specialized clinics or institutes for gastrointestinal disorders.
QUESTIONS TO ASK THE DOCTOR
Questions to ask the primary care physician:
- What are my alternatives?
- Is surgery the answer for me?
- Can you recommend a surgeon who performs the laparoscopic procedure?
- If surgery is appropriate for me, what are the next steps?
Questions to ask the surgeon:
- How many times have you performed Nissen or laparoscopic fundoplication?
- Are you a board-certified surgeon?
- What types of outcomes have you had?
- What are the most common side effects or complications?
- What should I do to prepare for surgery?
- What should I expect following the surgery?
- Can you refer me to one of your patients who has had this procedure?
- What type of diagnostic procedures are performed to determine if patients require surgery?
- Will I need to see another specialist for the diagnostic procedures?
- Do you use endoscopy, motility studies, and/ or pH studies for your pre-operative evaluation?
Your comments have helped me considerably. Guess I will really have to be cautious about eating in unclean-type restaurants, as the need to regurgitate sounds nearly impossible.
I was told there would be tubes inserted - kept in place after surgery, if necessary, for a while - to expel any gas or liquids that remain. Hopefully, I will be able to give up the proton pumps, because I already have osteopenia and do not wish to break a hip, etc.
My surgery was performed laparoscopically. I was in the hospital for four days. The doctors wanted to ensure that my bowels were functioning properly, so don't expect to leave until you can "prove it". The hospital gave me short term pain meds in conjunction with anti nausea medication. They didn't want me heaving and placing pressure on the procedure.
My Personal results:
1 Year: Be careful what you eat or drink, you can't vomit. If you do ingest something bad, be prepared for the dry heaves until it passes through your system. No reflux, no need for medication.
5 years: No reflux and no need for medications. A great overall improvement to quality of life.
7 years: Noticing a little reflux, but nothing in comparison to pre-surgery
10 years: Back on Protonix, 40mg twice per day. Can vomit again. Relocated to new city and can't find a GI doctor with experience in caring for or monitoring this procedure. Lesson learned: Keep a personal copy of your medical records if you relocate frequently.
Overall: It worked and was worth it for me even if only for 10 years.
Personal notes: Avoid alcohol, avoid nicotine, limit caffeine intake
given me alot of info and alot to think about.
In my case, the surgeon thought he had nicked the small bowel and put a stitch in what he could see to try and close the nick. I was then dispatched to recovery where I lay in increasing agony for some 6 hours before the surgeon reappeared to suggest I have a scan and and then see how things were the following day. Whilst I was being given increasing volumes of morphine to manage the increasingly excruciating pain in my abdomen, I managed to let hom know I felt there was a serious problem and that I would get through the night. I was taken back into theatre immediately where I was opened up and found to have a completely ruptured/severed small bowel which had been leaking profusely for circa 6 hours! The surgeon hadn't bothered to check the extent of damage during the initial procedure and this could easily have cost me my life. As someone involved in the legal profession myself, I can only interpret this as negligence at best if not gross negligence as he was well aware of the implications and he chose to disregard those through his initial reaction. I then developed a paralytic ileus which should have passed in 2/3 days but went on for 11 days. Rather than inserting an NGT, the medical staff chose to wait and see how things went...a week later, I was rushed back to theatre as I was in agony and there was a very real concern that my stomach was going to rupture. I had almost 5 litres of fluid removed and the surgeon has since told my family it could have waited another day, this despite the fact that the capacity of the stomach is circa 1.6 litres. Just to compound matters, the wound became infected and they simply took a scalpel to it and have left a gaping hole in the abdomen to heal itself...it will be very messy. I have also been left with a hugely distended abdomen and this for someone who had a very flat/toned abdomen the day I went in for the surgery.
The whole experience has been disastrous and I have yet to experience any benefit...perhaps I will in time but to date, all I've incurred has been incredible suffering and personal damage, attempted cover ups at every turn by the medical teams and potentially irreperable damage to my business (I'd been told I'd be in hospital for 2 days instead of the 3 weeks and that I'd be back working within a week rather than what will turn out to be 2 to 3 months). I'd strongly recommend anyone thinking about this surgery to question how essential it might be, what the alternatives are, what the implications are if something goes wrong and to thoroughly research the credentials and integrity of the surgeon/gastroenterologist. The decision to proceed and the problems encountered have damaged my life and detrimentally impacted on the quality of my future life.
My own NF wrap is 16 years old and still works like a charm. My surgeon used "Ethibond Excel" size "0" braided polyester sutures which maintain 100 percent tensile strength, indefinitely, in vivo.