Thoracotomy
Definition
Thoracotomy is the process of making of an incision (cut) into the chest wall.
Purpose
A physician gains access to the chest cavity (called the thorax) by cutting through the chest wall. Reasons for the entry are varied. Thoracotomy allows for study of the condition of the lungs; removal of a lung or part of a lung; removal of a rib; and examination, treatment, or removal of any organs in the chest cavity. Thoracotomy also provides access to the heart, esophagus, diaphragm, and the portion of the aorta that passes through the chest cavity.
Lung cancer is the most common cancer requiring a thoracotomy. Tumors and metastatic growths can be removed through the incision (a procedure called resection). A biopsy, or tissue sample, can also be taken through the incision, and examined under a microscope for evidence of abnormal cells.
A resuscitative or emergency thoracotomy may be performed to resuscitate a patient who is near death as a result of a chest injury. An emergency thoracotomy provides access to the chest cavity to control injury-related bleeding from the heart, cardiac compressions to restore a normal heart rhythm, or to relieve pressure on the heart caused by cardiac tamponade (accumulation of fluid in the space between the heart's muscle and outer lining).
Demographics
Thoracotomy may be performed to diagnose or treat a variety of conditions; therefore, no data exist as to the overall incidence of the procedure. Lung cancer, a common reason for thoracotomy, is diagnosed in approximately 172,000 people each year and affects more men than women (91,800 diagnoses in men compared to 80,100 in women).
Description
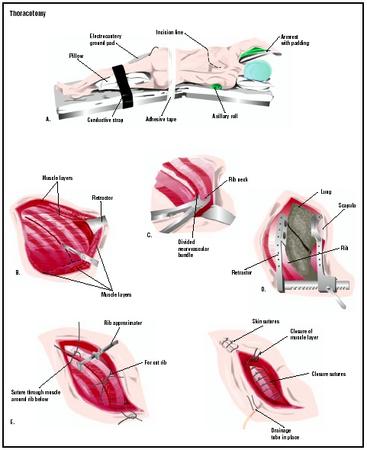
The thoracotomy incision may be made on the side, under the arm (axillary thoracotomy); on the front, through the breastbone (median sternotomy); slanting from the back to the side (posterolateral thoracotomy); or under the breast (anterolateral thoracotomy). The exact location of the cut depends on the reason for the surgery. In some cases, the physician is able to make the incision between ribs (called an intercostal approach) to minimize cuts through bone, nerves, and muscle. The incision may range from just under 5 in (12.7 cm) to 10 in (25 cm).
During the surgery, a tube is passed through the trachea. It usually has a branch to each lung. One lung is deflated for examination and surgery, while the other one is inflated with the assistance of a mechanical device (a ventilator).
A number of different procedures may be commenced at this point. A lobectomy removes an entire lobe or section of a lung (the right lung has three lobes and the left lung has two). It may be done to remove cancer that is contained by a lobe. A segmentectomy , or wedge resection, removes a wedge-shaped piece of lung smaller than a lobe. Alternatively, the entire lung may be removed during a pneumonectomy .
In the case of an emergency thoracotomy, the procedure performed depends on the type and extent of injury. The heart may be exposed so that direct cardiac compressions can be performed; the physician may use one hand or both hands to manually pump blood through the heart. Internal paddles of a defibrillating machine may be applied directly to the heart to restore normal cardiac rhythms. Injuries to the heart causing excessive bleeding (hemorrhaging) may be closed with staples or stitches.
Once the procedure that required the incision is completed, the chest wall is closed. The layers of skin, muscle, and other tissues are closed with stitches or staples. If the breastbone was cut (as in the case of a median sternotomy), it is stitched back together with wire.
Diagnosis/Preparation
Patients are told not to eat after midnight the night before surgery. The advice is important because vomiting during surgery can cause serious complications or death. For surgery in which a general anesthetic is used, the gag reflex is often lost for several hours or longer, making it much more likely that food will enter the lungs if vomiting occurs.
Patients must tell their physicians about all known allergies so that the safest anesthetics can be selected. Older patients must be evaluated for heart ailments before surgery because of the additional strain on that organ.
Aftercare
Opening the chest cavity means cutting through skin, muscle, nerves, and sometimes bone. It is a major procedure that often involves a hospital stay of five to seven days. The skin around the drainage tube to the thoracic cavity must be kept clean, and the tube must be kept unblocked.
The pressure differences that are set up in the thoracic cavity by the movement of the diaphragm (the large muscle at the base of the thorax) make it possible for the lungs to expand and contract. If the pressure in the chest cavity changes abruptly, the lungs can collapse. Any fluid that collects in the cavity puts a patient at risk for infection and reduced lung function, or even collapse (called a pneumothorax). Thus, any entry to the chest usually requires that a chest tube remain in place for several days after the incision is closed.
The first two days after surgery may be spent in the intensive care unit (ICU) of the hospital. A variety of tubes, catheters, and monitors may be required after surgery.
Risks
The rich supply of blood vessels to the lungs makes hemorrhage a risk; a blood transfusion may become necessary during surgery. General anesthesia carries such risks as nausea, vomiting, headache, blood pressure issues, or allergic reaction. After a thoracotomy, there may be drainage from the incision. There is also the risk of infection; the patient must learn how to keep the incision clean and dry as it heals.
After the chest tube is removed, the patient is vulnerable to pneumothorax. Physicians strive to reduce the risk of collapse by timing the removal of the tube. Doing so at the end of inspiration (breathing in) or the end of expiration (breathing out) poses less risk. Deep breathing exercises and coughing should be emphasized as an important way that patients can improve healing and prevent pneumonia.
Normal results
The results following thoracotomy depend on the reasons why it was performed. If a biopsy was taken during the surgery, a normal result would indicate that no cancerous cells are present in the tissue sample. The procedure may indicate that further treatment is necessary; for example, if cancer was detected, chemotherapy, radiation therapy, or more surgery may be recommended.
Morbidity and mortality
One study following lung cancer patients undergoing thoracotomy found that 10–15% of patients experienced heartbeat irregularities, readmittance to the ICU, or partial or full lung collapse; 5–10% experienced pneumonia or extended use of the ventilator (greater than 48 hours); and up to 5% experienced wound infection, accumulation of pus in the chest cavity, or blood clots in the lung. The mortality rate in the study was 5.8%, with patients dying as a result of the cancer itself or of postoperative complications.
Alternatives
Video-assisted thoracic surgery (VATS) is a less invasive alternative to thoracotomy. Also called thoracoscopy, VATS involves the insertion of a thoracoscope (a thin, lighted tube) into a small incision through the chest wall. The surgeon can visualize the structures inside the chest cavity on a video screen. Such instruments as a stapler or grasper may inserted through other small incisions. Although initially used as a diagnostic tool (to visualize the lungs or to remove a sample of lung tissue for further examination), VATS may be used to remove some lung tumors.
An alternative to emergency thoracotomy is a tube thoracostomy, a tube placed through chest wall to drain excess fluid. Over 80% of patients with a penetrating chest wound can be successfully managed with a thoracostomy.
See also ; Thoracoscopy .
Resources
books
Bartlett, Robert L. "Resuscitative Thoracotomy." (Chapter 17). In Clinical Procedures in Emergency Medicine. Philadelphia: W. B. Saunders Company, 1998.
Townsend, Courtney M., et al. "Thoracic Incisions." (Chapter 55). In Sabiston Textbook of Surgery. Philadelphia: W. B. Saunders Company, 2001.
periodicals
Blewett, C.J. et al. "Open Lung Biopsy as an Outpatient Procedure." Annals of Thoracic Surgery (April 2001): 1113-5.
Handy, John R., et al. "What Happens to Patients Undergoing Lung Cancer Surgery? Outcomes and Quality of Life Before and After Surgery." Chest 122, no.1 (August 14, 2002): 21-30.
Swanson, Scott J. and Hasan F. Batirel. "Video-Assisted Thoracic Surgery (VATS) Resection for Lung Cancer." Surgical Clinics of North America 82, no.3 (June 1, 2002): 541-9.
organizations
American Cancer Society. 1599 Clifton Rd. NE, Atlanta, GA 30329-4251. (800) 227-2345. http://www.cancer.org .
Society of Thoracic Surgeons. 663 N. Saint Clair St., Suite 2320, Chicago, IL 60611-3658. (312) 202-5800. http://www.sts.org .
other
"Detailed Guide: Lung Cancer." American Cancer Society. [cited April 28, 2003]. http://www.cancer.org/docroot/CRI/CRI_2_3x.asp?dt=26 .
Diane M. Calabrese Stephanie Dionne Sherk
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Thoracotomy may be performed by a thoracic surgeon, a medical doctor who has completed surgical training in the areas of general surgery and surgery of the chest area, or an emergency room physician (in the case of emergency thoracotomy). The procedure is generally performed in a hospital operating room , although emergency thoracotomies may be performed in an emergency department or trauma center.
QUESTIONS TO ASK THE DOCTOR
- Why is thoracotomy being recommended?
- What diagnostic tests will be performed to determine if thoracotomy is necessary?
- What type of incision will be used and where will it be located?
- What type of procedure will be performed?
- How long will is the recovery time and what is expected during this period?
- If a biopsy is the only reason for the procedure, is a thoracoscopy or a guided needle biopsy an option (instead of thoracotomy)?
Very good article. Thanks.
Thank you. Excellent article!
I had these when I was 58, and it took me awhile to fully recover. Even though I lost 40% of my lungs, I have hiked and worked out and learned to breath a little differently. (Breath in through nose and then out through pursed lips - this maximizes exchange of O2 to take place).
About healing--it took me more than a year to get where I began to feel comfortable. But right from the start, I began walking and slowly increased my distances. I found that using a pedometer to keep track was helpful and after two years was logging about 600 miles a year. This also presented a challenge to me and gave me focus to push on.
I have recently had some heart issues and am now wondering if the extra hard breathing I have had to do while hiking/climbing has caused some of these issues. Docs are looking into it. So, wishing luck to each of you!
Marge
They made 3 incisions: 1 for the scope - 1 for the chest tube -and one in the crease under my right breast. I was originally told I would be in the hospital for 5 days - they made me leave less than 24 hours later even though I said I wasn't comfortable going home yet.
Anyways, I found that all of the pain I was experiencing was where the chest tube had run under my breast. 11 days later I'm still highly dependant on my painkillers and even they don't take the pain away half the time! I can't wear my bra so I've been walking around basically holding my boob up so the weight isn't on the area where it hurts. It's unbearable.
Has anyone else had this much pain from the chest tube??
AFTER THE OP I WAS MANAGED WITH AN EPIDURAL.GREAT RELIEF OF PAIN.
WHEN THE EPIDURAL WAS REMOVED THERE WAS A GREAT DEAL OF PAIN BUT WAS MANAGED WITH PAIN MEDS.
FOUND I WAS VERY WEAK WHEN DISCHARGED HOME.DOING BREATHING EXERCISES AND MOVING MORE EVERYDAY.FIND I HAVE STRANGE SHARP PAINS NOW AND AGAIN.CANNOT DO ALL I WANT TO DO,VERY FRUSTRATING.
I LIVE IN SAUDI ARABIA AND I AM FLYING TO LONDON TO DO THE( WALK FOR LIFE )ON THE 7TH OF MAY FOR MY FRIENDS WHO ARE SUFFERING THE SAME DISEASE.
WISH ME LUCK
J
lung in January of 2011. I HAVE HEALED WELL EVEN THOUGH I turned 73 years of age yesterday. I did not really go back and talk to my surgeon after the surgery healed as it was a trip I did not feel able to make on my own and I did not want to ask my brother to drive me. I am still finding it necessary to take some prescription pain med, and in fact went to the grocery store last evening and bought two 20 lb bags of ice as well as a rather large water melon. When I got out of bed this morning I noticed fairly substantial pain under right arm, and under my right breast where I understand that this is where the incision was made (scars bear that out)and possibly ribs were spread in the area under the right breast. I assume what I am experiencing is pain as a result of heavy lifting. Should I feel concern that I could have damaged other surgery tissue, etc
38 years of age. I am now 41 and have been dealing with this for over 3 years. The DRS still have no idea what has caused this issue. My samples were sent and tested at the Mayo Clinic. I am
now taking a Chemo medication that seems to be helping. I wasn't aware that this procedure would be so invassive. I still have movement issues and sometimes it hurts to take a breath. Anyone that is having this done--make sure to stretch and use the tube to measure the pressure in your breaths it will help eventually. May God Bless you all and speedy recovers.
Good luck to everyone.
I'm happy all of you got your operations I'm sorry it's been a tuff road ahead for some of you but I thank G-d you made it and your still here!
Not so.. For my husband who suffered horribly with a intercostal muscle hemmorage and wasn't propererly given the right medical advice and everything went wrong.. I stumbled upon your discussion and this looks like this would have been the operation he needed.. To get better.. He walked around with that excurting pain for 2 yrs and died of narcotic od in sept.. Such a loss so sad..
Happy Holidays.. Your going to be ok:)
Sorry for your loss~ I know, I will never feel normal again, I will be in constant discomfort, maybe it's better to be dead than alive, and suffer your whole life !!
God Bless, Happy Holidays !!
I feel as if my surgeon did not really tell me the recovery time as I was taken in the day after my appointment in clinic. Always ask questions!! That I must stress!
Good luck to all having this surgery!
I am quite keen to get back at the gym properly I started back second week of January doing light weights! I started doing my chest again this week! I am way down on weights from doing 30kg in each arm to 16kgs! Of course I want to be mindful of the healing process! Thanks in advance! Jake
I had been given a thoracotomy after two weeks as I had gone into total respiratory failure and was on a ventilator, I haven't worked since but am just feeling I may be able to do light work now, I get very exhausted and still have a lot of pain in Lung, have had ultrasound on wound which did help and do physio every day, parts of breast and back are still numb and I think will always be, movement in arm limited and if I lift a heavy object know about it day after!! Still alive though !!
We recently got him on Morphine after Vicodine after surgery. He is still having bad pain especially at night and not able to sleep. I really hate to hear this might take a year to get some comfort, he is getting in the sucidal mood. Doc just keep saying you will hurt for a while but no indication of how long.
I woke up 3 days later in ICU and under quarantine for TB (which turned out to be negative) tubes in my side and huge incision and plenty of pain to go around. The pain meds that were introduced then did help to a large degree, making it tolerable so long as I remained on schedule with them. Lot's of nutrition and fluids through the IV, daily blood thinner shots in the belly, breathing treatments and daily xrays rounded out the routine. After a week total in ICU, they ruled out the TB and moved me to a regular room where I continued to improve daily. The tubes were removed this past Thursday and I was discharged on Friday June 01 never knowing what procedures were performed on me (by their proper name) and asked on Monday.
I came across this article looking up the technical terms and wow am I shocked. I had no idea that this was so serious (though I did know it is/was painful). The lady who said that this is the worse pain she has ever known including childbirth is right on the money! Without the morphine and fentnyl, the pain would be unbareable! I feel so bad (and even guilty)for a lot of you guys who seem to be stagnant (or worse) in recovery as I seem to be getting to feeling better everyday. I hope that I will be better soon but, after reading all of your stories, I will take my time with it. Best wishes to each of you and yours and God Bless us all.
I was diagnosed with pneumonia at Thanksgiving of 2011.
In January 2012, I was admitted to the hospital. I had a Posterolateral Thoracotomy on February 14, 2102 to remove material from my right lung to be able to run tests on the material to try and diagnos my condition. I was in the hospital for 25 days and was released 3 days after the Thoracotomy on 17 February. I have been on every kind of antibiotic known to man with no improvement. I returned to the hospital in May 2012 for another 16 days or so because I could not breathe. My Pulmonologist finally diagnosed me with Cryptogenic Organizing Pneumonia (COP). I then went to Duke University Medical Clinic to verify the diagnosis and to see if they could figure out what to do for me.
It seems that my immune system attacked itself and caused my right lung to fill with white cells. Breathing has been very difficult. I am now off of the antibiotics cause the doctors say it's not viral or bacterial. I am now on steroids which seems to be allowing my body to return to a semblance of normality. I hope and pray that in 30 days or so, the doc will reduce the amount of steroids and then in another 30 days reduce the amount even more and sometime after that to be off of them all together.
The recovery from the Posterolateral Thoracotomy has been a bear! It's been about 85 days since the surgery. My right side (rib cage) is still numb and tender and swollen. I have an 8.5 inch scar on my back and a scar on my right rib cage where the drain tube was located. Range of motion seems ok, but after mild activity, the area under the scar on my back sems to sweel. I get a swollen feeling and tenderness about the size of half a racketball. I am off of the pain meds except for some moltrin which seems to take care of most of my pain and some inflamation.
My doctor did not tell me that I would have over 4 months of recovery. I found this out a month after my surgery. My family doctor, my pumonologist and my infectious disease doctor thought I would have 3 small incisions near my rib cage and not the major incision that I did have. I also found out from the doctor at Duke that the surgeon did not take enough material from the right places in the lung.
Make sure your doctor/surgeon explains everything to you before you give permission to him/her to cut on you!
I'm a 38 year old male with good fitness. The surgery was the result of a two month process of too many collapsed lungs, chest tubes, ER and hospital visits and a video assisted thoracotomy that did not resolve the lung leaking air. Once the posterolateral thoracotomy happened, and Valley Fever was found to be the culprit, it was the start of resolution.
The hospital stay should have been a week, but I spent 3 weeks with the complication of kidney failure due to blood loss during surgery. The pain was definitely there, I couldn't have the standard epidural with the then unknown infection because of the possibility of developing meningitis. So, morphine, dilaudid and then percocets were the routine for the ensuing 2 weeks after surgery. I was up and pacing around the halls of the hospital within days. Slow progress continued from walks around the block to where I was taking 7-10 mile bicycle rides in a month and a half after surgery. The bike is great due the lack of impact, any exercise or any thing at all bumpy or remotely resembling an impact will bring pain. The percocets continue as needed, I have taken 24 since leaving the hospital six months ago.
The healing of the access points is the long term annoyance. The back scar and the under the skin scarring where the surgeon went into the chest cavity from the front are still not normal - tenderness and numbness there. I have been told it could take a year or more to feel normal. There is so much healing to be done with this surgery. Consider all of the muscle, nerves and bone that has to be cut through. I am six months on from surgery and have some tightness in the muscles on the side of surgery, and occasionally a little pain with prolonged sitting in certain positions or too much exercise. I measure the progress in months. Day to day it feels the same, but month to month there is notable improvement in range of motion, strength and pain. Patience is the key.
The best bit of advice I heard was from a nurse, be involved with the process. Ask questions and be informed about what is going on - it reduces the chance of mistakes by hospital staff, plus it keeps you from feeling helpless and in the dark.
In all honesty it hurts a lot. I talking about excruciating pain one they take the pump out and switch you to morphine shots and hydrocodone. I found that it takes at least 10 mg every 5 hours for pain and that means if you wait six hours you wake up very painful, This is the reason someone should wake you up to take at least one pain pill. They will not normally send you home with morphine in tablet form and suspect you want the drugs to get high; however, once I took all the ones I had and was released from the surgeon my oncologist said she would up the dosage to 10 mg and take two if I need them as often as I need them and gave me two months worth. after a couple days of taking regular dosages of pain pills, you get to sleep a little more unless you role over to the effective side which wakes you up. A cough of any magnitude will wake you from the dead for about 1.5 months. You find that a sneeze is more painful, and keep in mind that you will probably get constipated. I thought nothing could get worse until I started this new drug Zelboraf for Melanoma. Just finished 1 nd 1/2 weeks and rash broke out all over and I itch like a wild man the dived naked into a bush of poison ivory. Just got told to cut the dosage in half and rubs lots of any medication that works externally and take lots of benadryl. Since it took a week to flare up it may take longer to dissipate. I hope it works, it is the only medication specifically for my condition with the least side effects. Anything has to be better than cutting another lung or part of it out. I hope this helps some of you.
I was in hospital for 7 nights due to my lung collapsing due to the chest drain being taken out to early
I wasn't expecting how much the pain would be but planning a pain medication plan would be benifical.
After the hospital stay I stayed at home for a week and then after that week started to feel better and went to see friends
But I was on mrophine and OxyContin painkillers for around 2 months after the operation.
I didn't play sport until the September but I did start ridimg my horse again 1 month after the operation.
I did think whilst I was in hospital that the operation wasn't worth how much
Pain I was in, but as I looks back on it now I am so happy I did it now !!!
I hope this helps anyone who is due to or thinking of having this surgery
As far as lasting side effects, I have trouble with shortness of breath when climbing and running. I use the breath in through nose, out through mouth technique. I still have pain on my side and still can't sleep on my back. Early on, I had the weird nerve issue where I would scratch my chest and feel it in my arm, but that subsided in about a year. I did some research on the web and found that about 33% have chronic pain afterward. After a while you learn to live with it.
After a year, I resumed all normal activity and worked out at the gym without issues except for the shortness of breath. Follow-up CT scans show extensive scaring in that area of the chest.
Make sure your pain is under control BEFORE you leave the hospital ( which is where I went wrong I think. Pain is more frightening when your home and no one to tell it's unbearable or know if it's normal) Good luck to all heading down this path.
Thanks
but to read this was kinda shocking to me. My boyfriend has cancer which has spread to his lungs, he has had this surgery three times now, the third time being today. I'm going to visit him in three days and I'm kind of nervous for that, I'm afraid he'll be in a lot of pain and I don't really know how to deal with that. His father messaged me that everything went as it should and that he is breathing on his own, but I still don't really know what to expect.
but to read this was kinda shocking to me. My boyfriend has cancer which has spread to his lungs, he has had this surgery three times now, the third time being today. I'm going to visit him in three days and I'm kind of nervous for that, I'm afraid he'll be in a lot of pain and I don't really know how to deal with that. His father messaged me that everything went as it should and that he is breathing on his own, but I still don't really know what to expect.
anaesthetic . I am now 14 days after my surgery and still have pain , even though it is not as bad. Just to let people know that you can have the same operation but the pain is different for every procedure. It does not go that because you had pain once that this will be the case every time.
Love the winter tires content on your site! You know, businesses get traffic from their blogs, and we feel that you could use a little help, since you are not blogging weekly yet.
Writing takes a lot of time and effort, and we have just the team to come up with great content you are looking for.
You can have a brand new article to post on surgeryencyclopedia.com starting at $10 in as little as 5 days!
Check out our work and reviews here: https://goo.gl/KGRAi4
Thanks for your time,
Enjoy the rest of your day.
Gus
Questions? Gus@seowriters.ml
You are receiving this email because the contact form at surgeryencyclopedia.com is open to the public.
If you like to opt-out of future communications from us, please submit your request here:
https://goo.gl/u4rPbG Unsubscribe to stop getting our emails.