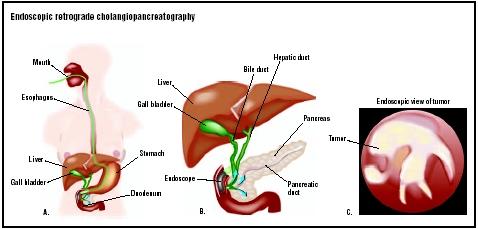
Endoscopic retrograde cholangiopancreatography
Definition
Endoscopic retrograde cholangiopancreatography (ERCP) is an imaging technique used to diagnose diseases of the pancreas, liver, gallbladder, and bile ducts. It combines endoscopy and x-ray imaging.
Purpose
ERCP is used in the management of diseases that affect the gastrointestinal tract, specifically the pancreas, liver, gall bladder, and bile ducts. The pancreas is an organ that secretes pancreatic juice into the upper part of the intestine. Pancreatic juice is composed of specialized proteins that help to digest fats, proteins, and carbohydrates. Bile is a substance that helps to digest fats; it is produced by the liver, secreted through the bile ducts, and stored in the gallbladder. Bile is released into the small intestine after a person has eaten a meal containing fat.
A doctor may recommend ERCP if a patient is experiencing abdominal pain of unknown origin, weight loss, or jaundice. These may be symptoms of biliary disease. For instance, gallstones that form in the gallbladder or bile ducts may become stuck there, causing cramping or dull pain in the upper right area of the abdomen, fever, and/or jaundice. Other causes of biliary obstruction include tumors, injury from gallbladder surgery, or inflammation. The bile ducts may also become narrowed (called a biliary stricture) as a result of cancer, blunt trauma to the abdomen, pancreatitis (inflammation of the pancreas), or primary biliary cirrhosis (PBC). PBC may be caused by a condition called primary sclerosing cholangitis, an inflammation of the bile ducts that may cause pain, jaundice, itching, or other symptoms. These symptoms may also be experienced by a patient with cholangitis, or with infection of the bile ducts caused by bacteria or parasites.
ERCP can also be used to diagnose a number of pancreatic disorders. Pancreatitis is an inflammation of the pancreas, caused by chronic alcohol abuse, injury, obstruction of the pancreatic ducts (e.g., by gallstones), or other factors. The condition may be either acute (having a severe but short course) or chronic (persistent). Symptoms of pancreatitis
creatitis include abdominal pain, weight loss, nausea, and vomiting. ERCP may be used to diagnose cancer of the pancreas; pancreatic pseudocysts (collections of pancreatic fluid); or strictures of the pancreatic ducts. Certain congenital disorders may also be identified by ERCP, such as pancreas divisum, a condition in which parts of the pancreas fail to fuse together during fetal development.
Demographics
Diseases of the pancreas and biliary tract affect millions of Americans each year. According to the National Health and Nutrition Survey, gallbladder disease affects approximately 6.3 million men and 14.2 million women in the United States between the ages of 24 and 74. Approximately one million new cases of gallstones are diagnosed each year. The incidence of gallstones is higher among women; adults over the age of 40; and people who are overweight. Primary sclerosing cholangitis occurs at a rate of two to seven cases per 100,000 persons. The rate of gallbladder cancer is approximately 2.5 out of 100,000 persons. In addition, approximately 87,000 cases of pancreatitis and 30,000 cases of pancreatic cancer are diagnosed each year in the United States.
Description
ERCP is performed with the patient given either a sedative or general anesthesia. The physician then sprays the back of the patient's throat with a local anesthetic. The endoscope (a thin, hollow tube attached to a viewing screen) is then inserted into the mouth. It is threaded down the esophagus, through the stomach, and into the duodenum (upper part of the small intestine) until it reaches the spot where the bile and pancreatic ducts empty into the duodenum. At this point a small tube called a cannula is inserted through the endoscope and used to inject a contrast dye into the ducts. The term "retrograde" in the name of the procedure refers to the backward direction of the dye as it is injected through the ducts. A series of x rays are then taken as the dye moves through the ducts.
If the x rays show that a problem exists, ERCP may be used as a therapeutic tool. Special instruments can be inserted into the endoscope to remove gallstones, take samples of tissue for further examination (e.g., in the case of suspected cancer), or place a special tube called a stent into a duct to relieve an obstruction.
Diagnosis/Preparation
ERCP is generally not performed unless other less invasive diagnostic tests have first been used to determine the cause of a patient's symptoms. Such tests include:
- complete medical history and physical examination
- blood tests (certain diseases can be diagnosed by abnormal levels of blood components)
- ultrasound imaging (a procedure that uses high-frequency sound waves to visualize structures in the human body)
- computed tomography (CT) scan (an imaging device that uses x rays to produce two-dimensional cross-sections on a viewing screen)
Before undergoing ERCP, the patient will be instructed to refrain from eating or drinking for at least six hours to ensure that the stomach and upper part of the intestine are empty. Arrangements should be made for someone to take the patient home after the procedure, as he or she will not be able to drive. The physician should also be given a complete list of all prescription, over-thecounter, and alternative medications or preparations that the patient is taking. The patient should also notify the doctor if he or she is allergic to iodine because the contrast dye contains it.
Aftercare
After the procedure, the patient will remain at the hospital or outpatient facility until the effects of the sedative wear off and no signs of any complications have appeared. A longer stay may be warranted if the patient experiences complications or if other procedures were performed.
Risks
Complications that have been reported with ERCP include pancreatitis, cholangitis (inflammation of the bile ducts), cholecystitis (inflammation of the gallbladder), injury to the duodenum, pain, bleeding, infection, and formation of blood clots. Factors that increase the risk of complications include liver damage, bleeding disorders, a history of post-ERCP complications, and a less experienced endoscopist.
Normal results
Following ERCP, the patient's biliary and pancreatic ducts should be free of stones and show no strictures, obstructions, or evidence of infection or inflammation.
Morbidity and mortality rates
The overall complication rate associated with ERCP is approximately 11%. Pancreatitis may occur in up to 7% of patients. Cholangitis and cholecystitis occur in less than 1% of patients. Infection, injury, bleeding, and blot clot formation also occur in less than 1%. The mortality rate for ERCP is approximately 0.1%.
Alternatives
Although less invasive techniques exist (such as computed tomography and ultrasonography) to help to diagnose gastrointestinal diseases, these imaging studies are often not precise enough to allow for definite diagnosis of certain conditions. Percutaneous transhepatic cholangiography (PTCA) is an alternative to ERCP that involves the insertion of a long, flexible needle through the skin to the bile ducts; contrast dye is then injected into the ducts so that they may be visualized by x ray. PTCA may be recommended if ERCP fails or cannot be performed. Magnetic resonance cholangiopancreatography (MRCP) is an imaging technology that allows for noninvasive examination of the biliary and pancreatic ducts. Its disadvantage, however, is that unlike ERCP, it cannot be used for therapeutic procedures as well as imaging.
Resources
books
Feldman, Mark, et al. Sleisenger & Fordtran's Gastrointestinal and Liver Disease , 7th ed. Philadelphia: Elsevier Science, 2002.
periodicals
Ahmed, Aijaz, and Emmet B. Keeffe. "Gallstones and Biliary Tract Disease." WebMD Scientific American Medicine February 28, 2003 [cited April 7, 2003]. http://www.medscape.com/viewarticle/449563_1 .
Aronson, Naomi, Carole Flamm, Rhonda L. Bohn, et al. "Evidence-Based Assessment: Patient, Procedure, or Operator Factors Associated with ERCP Complications." Gastrointestinal Endoscopy 56, no. 6 (December 2002)(6 Suppl): S294-S302.
Freeman, Martin L. "Adverse Outcomes of ERCP." Gastrointestinal Endoscopy 56, no. 6 (December 2002) (6 Suppl): S273-S282.
Vandervoort, Jo, et al. "Risk Factors for Complications After Performance of ERCP." Gastrointestinal Endoscopy 56, no. 5 (November 2002): 652-656.
Yakshe, Paul. "Biliary Disease." eMedicine , March 29, 2002 [cited April 7, 2003]. http://www.emedicine.com/MED/topic 225.htm .
Yakshe, Paul. "Pancreatitis, Chronic." eMedicine , January 8, 2003 [cited April 7, 2003]. http://www.emedicine.com/med/topic1721.htm .
organizations
American College of Gastroenterology. 4900 B South 31st St., Arlington, VA 22206. (703) 820-7400. http://www.acg.gi.org .
American Gastroenterological Association. 7910 Woodmont Ave., 7th Floor, Bethesda, MD 20814. (301) 654-2055. http://www.gastro.org .
American Society for Gastrointestinal Endoscopy. 1520 Kensington Rd., Suite 202, Oak Brook, IL 60523. (630) 573-0600. http://www.asge.org .
other
National Digestive Diseases Information Clearinghouse. Endoscopic Retrograde Cholangiopancreatography. Bethesda, MD: NDDIC, 2002. [cited April 7, 2003]. http://www.niddk.nih.gov/health/digest/pubs/diagtest/ercp.htm .
Stephanie Dionne Sherk
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
ERCP is usually performed in the x-ray department of a hospital or outpatient facility by a gastroenterologist, a medical doctor who has completed specialized training in the diagnosis and treatment of diseases of the digestive system. An anesthesiologist administers the anesthetic, and a radiologist may be consulted in interpreting the images obtained by the dye injection.
QUESTIONS TO ASK THE DOCTOR
- Why is ERCP recommended in my case?
- What diagnostic tests will be performed prior to ERCP?
- How long will the procedure take?
- When will I find out the results?
- Will you treat the problem if one is found during the procedure?
Make sure you are not allergic to it, like I am
a week, while they tried to figure out what the problem was. They did many different scans! Finally they saw there was bile in her abdomen. They did a ERCP procedure, found the sepage from the bile duct and repaired it, they put a
stent to direct the bile into the small intestine. Also, took care of the Iilias (narrowing of the small intestine muscle) which had developed scaring! Once this
was over, she felt instant relief! Her nausea is now gone, the pain is as intense or constant! It's been 3 days, she now feels, a different sharp, tearing pain under her right breast, but isn't constant as before! She has major temps tire body changes, shivers from feeling too cold & then gets too hot, yet her tempature reading is normal! The
meds manage the pain for about 3-4 hours! Is this normal or should she go back to the hospital? It's been 3 days since this procedure!