Colostomy
Definition
A colostomy is a surgical procedure that brings a portion of the large intestine through the abdominal wall to carry feces out of the body.
Purpose
A colostomy is a means to treat various disorders of the large intestine, including cancer, obstruction, inflammatory bowel disease, ruptured diverticulum, ischemia (compromised blood supply), or traumatic injury. Temporary colostomies are created to divert stool from injured or diseased portions of the large intestine, allowing rest and healing. Permanent colostomies are performed when the distal bowel (at the farthest distance) must be removed or is blocked and inoperable. Although colorectal cancer is the most common indication for a permanent colostomy, only about 10–15% of patients with this diagnosis require a colostomy.
Demographics
Estimates of all ostomy surgeries (those involving any opening from the abdomen for the removal of either feces or urine) range from 42,000 to 65,000 each year; about half are temporary. Emergency surgeries for bowel obstruction and/or perforation comprise 10–15% of all colorectal surgeries; a portion of these result in colostomy.
Description
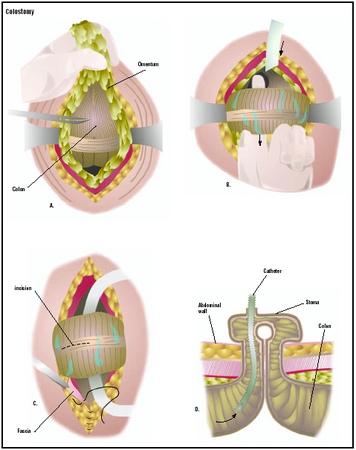
Surgery will result in one of three types of colostomies:
- End colostomy. The functioning end of the intestine (the section of bowel that remains connected to the upper gastrointestinal tract) is brought out onto the surface of the abdomen, forming the stoma (artificial opening) by cuffing the intestine back on itself and suturing the end to the skin. The surface of the stoma is actually the lining of the intestine, usually appearing moist and pink. The distal portion of bowel (now connected only to the rectum) may be removed, or sutured closed and left in the abdomen. An end colostomy is usually a permanent ostomy, resulting from trauma, cancer, or another pathological condition.
- Double-barrel colostomy. This involves the creation of two separate stomas on the abdominal wall. The proximal (nearest) stoma is the functional end that is connected to the upper gastrointestinal tract and will drain stool; the distal stoma, connected to the rectum and also called a mucous fistula, drains small amounts of mucus material. This is most often a temporary colostomy performed to rest an area of bowel, and to be later closed.
- Loop colostomy. This surgery brings a loop of bowel through an incision in the abdominal wall. The loop is held in place outside the abdomen by a plastic rod slipped beneath it. An incision is made in the bowel to allow the passage of stool through the loop colostomy. The supporting rod is removed approximately seven to 10 days after surgery, when healing has occurred that will prevent the loop of bowel from retracting into the abdomen. A loop colostomy is most often performed for creation of a temporary stoma to divert stool away from an area of intestine that has been blocked or ruptured.
Diagnosis/Preparation
A number of diseases and injuries may require a colostomy. Among the diseases are inflammatory bowel disease and colorectal cancer. Determining whether this surgery is necessary is a decision the physician makes based on a number of factors, including patient history, amount of pain, and the results of tests such as colonoscopy and lower G.I. (gastrointestinal) series. Due to lifestyle impact of the surgery, the decision is made after careful consultation with the patient. However, an immediate decision may be made in emergency situations involving injuries or puncture wounds in the abdomen or intestinal perforations related to diverticulear disease, ulcers, or life-threatening cancer.
As with any surgical procedure, the patient will be required to sign a consent form after the procedure is explained thoroughly. Blood and urine studies, along with various x rays and an electrocardiograph (EKG), may be ordered as the doctor deems necessary. If possible, the patient should visit an enterostomal therapist, who will mark an appropriate place on the abdomen for the stoma and offer preoperative education on ostomy management.
In order to empty and cleanse the bowel, the patient may be placed on a low-residue diet for several days prior to surgery. A liquid diet may be ordered for at least the day before surgery, with nothing by mouth after midnight. A series of enemas and/or oral preparations (GoLytely or Colyte) may be ordered to empty the bowel of stool. Oral anti-infectives (neomycin, erythromycin, or kanamycin sulfate) may be ordered to decrease bacteria in the intestine and help prevent postoperative infection. A nasogastric tube is inserted from the nose to the stomach on the day of surgery or during surgery to remove gastric secretions and prevent nausea and vomiting. A urinary catheter (a thin plastic tube) may also be inserted to keep the bladder empty during surgery, giving more space in the surgical field and decreasing chances of accidental injury.
Aftercare
Postoperative care for the patient with a new colostomy, as with those who have had any major surgery, involves monitoring of blood pressure, pulse, respirations, and temperature. Breathing tends to be shallow because of the effect of anesthesia and the patient's reluctance to breathe deeply and experience pain that is caused by the abdominal incision. The patient is instructed how to support the operative site during deep breathing and coughing, and given pain medication as necessary. Fluid intake and output is measured, and the operative site is observed for color and amount of wound drainage. The nasogastric tube will remain in place, attached to low, intermittent suction until bowel activity resumes. For the first 24–48 hours after surgery, the colostomy will drain bloody mucus. Fluids and electrolytes are infused intravenously until the patient's diet can gradually be resumed, beginning with liquids. Usually within 72 hours, passage of gas and stool through the stoma begins. Initially, the stool is liquid, gradually thickening as the patient begins to take solid foods. The patient is usually out of bed in eight to 24 hours after surgery and discharged in two to four days.
A colostomy pouch will generally have been placed on the patient's abdomen around the stoma during surgery. During the hospital stay, the patient and his or her caregivers will be educated on how to care for the colostomy. Determination of appropriate pouching supplies and a schedule of how often to change the pouch should be established. Regular assessment and meticulous care of the skin surrounding the stoma is important to maintain an adequate surface on which to attach the pouch. Some patients with colostomies are able to routinely irrigate the stoma, resulting in regulation of bowel function; rather than needing to wear a pouch, these patients may only need a dressing or cap over their stoma. Often, an enterostomal therapist will visit the patient in the hospital or at home after discharge to help the patient with stoma care.
Dietary counseling will be necessary for the patient to maintain normal bowel function and to avoid constipation, impaction, and other discomforts.
Risks
Potential complications of colostomy surgery include:
- excessive bleeding
- surgical wound infection
- thrombophlebitis (inflammation and blood clot to veins in the legs)
- pneumonia
- pulmonary embolism (blood clot or air bubble in the lungs' blood supply)
Psychological complications may result from colostomy surgery because of the fear of the perceived social stigma attached to wearing a colostomy bag. Patients may also be depressed and have feelings of low self-worth because of the change in their lifestyle and their appearance. Some patients may feel ugly and sexually unattractive and may worry that their spouse or significant other will no longer find them appealing. Counseling and education regarding surgery and the inherent lifestyle changes are often necessary.
Normal results
Complete healing is expected without complications. The period of time required for recovery from the surgery may vary depending on the patient's overall health prior to surgery and the patient's willingness to participate in stoma care. The colostomy patient without other medical complications should be able to resume all daily activities once recovered from the surgery. Adjustments in diet and daily personal care will need to be made.
Morbidity and mortality rates
Complications after colostomy surgery can occur. The doctor should be made aware of any of the following problems after surgery:
- increased pain, swelling, redness, drainage, or bleeding in the surgical area
- headache, muscle aches, dizziness, or fever
- increased abdominal pain or swelling, constipation, nausea or vomiting, or black, tarry stools
Stomal complications can also occur. They include:
- Death (necrosis) of stomal tissue. Caused by inadequate blood supply, this complication is usually visible 12–24 hours after the operation and may require additional surgery.
- Retraction (stoma is flush with the abdomen surface or has moved below it). Caused by insufficient stomal length, this complication may be managed by use of special pouching supplies. Elective revision of the stoma is also an option.
- Prolapse (stoma increases length above the surface of the abdomen). Most often this results from an overly large opening in the abdominal wall or inadequate fixation of the bowel to the abdominal wall. Surgical correction is required when blood supply is compromised.
- Stenosis (narrowing at the opening of the stoma). Often this is associated with infection around the stoma or scarring. Mild stenosis can be removed under local anesthesia; severe stenosis may require surgery for reshaping the stoma.
- Parastomal hernia (bowel causing bulge in the abdominal wall next to the stoma). This occurs due to placement of the stoma where the abdominal wall is weak or an overly large opening in the abdominal wall was made. The use of an ostomy support belt and special pouching supplies may be adequate. If severe, the defect in the abdominal wall should be repaired and the stoma moved to another location.
Mortality rates for colostomy patients vary according to the patient's general health upon admittance to the hospital. Even among higher risk patients, mortality is about 16%. This rate is greatly reduced (between 0.8% and 3.8%) when the colostomy is performed by a board-certified colon and rectal surgeon.
Alternatives
When a colostomy is deemed necessary, there are usually no alternatives to the surgery, though there can be alternatives in the type of surgery involved and adjuvant therapies related to the disease. For example, laparoscopic surgery is being used with many diseases of the intestinal tract, including initial cancers. For this surgery, the colon and rectal surgeon inserts a laparoscope (an instrument that has a tiny video camera attached) through a small incision in the abdomen. Other small incisions are made for the surgeon to insert laparoscopic instruments to use in creating the colostomy. This surgery often results in a shorter stay in the hospital, less postoperative pain, a quicker return to normal activities, and far less scarring. It is not recommended for patients who have had extensive prior abdominal surgery, large tumors, previous cancer, or serious heart problems.
Resources
books
Doughty, Dorothy. Urinary and Fecal Incontinence. St. Louis: Mosby-Year Book, Inc., 1991.
Hampton, Beverly, and Ruth Bryant. Ostomies and Continent Diversions. St. Louis: Mosby-Year Book, Inc., 1992.
Monahan, Frances. Medical-Surgical Nursing. Philadelphia: W. B. Saunders Co., 1998.
organizations
United Ostomy Association, Inc. (UOA). 19772 MacArthur Blvd., Suite 200, Irvine, CA 92612-2405. (800) 826-0826. http://www.uoa.org .
Wound Ostomy and Continence Nurses Society. 2755 Bristol Street, Suite 110, Costa Mesa, CA 92626. (714) 476-0268. http://www.wocn.org .
other
National Digestive Diseases Information Clearinghouse. Ileostomy, Colostomy, and Ileoanal Reservoir Surgery. (February 1, 2000): 1.
Janie F. Franz Kathleen D. Wright, RN
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
General surgeons and colon and rectal surgeons perform colostomies as inpatient surgeries, under general anesthesia.
QUESTIONS TO ASK THE DOCTOR
- What kinds of preoperative tests will be required?
- What drugs will be given for pain after the surgery?
- What will I need to do to prepare for surgery?
- Is there an enterostomal therapist I can talk to before the surgery?
- What will my recovery time be and what restrictions will I have?
- Is there an ostomy support group at the hospital that I can attend?
thanking you
I wish the article would have mentioned a little more concerning depression as attitude is very important in recovery. My colostomy is permanant. Accepting that and planning my activities to be prepared has allowed me to feel better about life. I have an excellent wife and family that have helped me very much.
There are many very unpleasant things that happen, concerning colostomies. Mucous discharge from the rectum is one. It usually last a week or less for me, but does put a damper on activities.
Thank you for all the great information.
thanking you
Any ideas on what causes the stoma bag to remain in black blood and not work at all following surgery? and how else is it possible to stop the bleeding? any idea?
At the age of 77 and with a history of diverticulitis
And over the past three years uc and many tests and scans etc a section was done and now have a colostomy bag. This was over two weeks ago but als the surgeon fitted a mucus drain fistula bag and said this would take two weeks to finish but still having the greenish mucus from there. I was wondering if anyone had the same or if indeed this took or will take longer?
At the age 25 2014 i had rectum canser after 1 year i had colostomi bag for 1 year this experience horrible but then to pass way after closeing bag now more diffiucult to manage moition problem now if i have to go out then i need to do fasting if any one can help in this stiution how to do
I had this checked by the Surgeon, who told me this is caused by granuloma. Since I had a colonoscopy done last year that gave me all clear, he was not worried about ant cancer risk. I also noticed that the size of the external circumference of the stoma has increased by almost 1 inch
But I am worried that this blood+mucus discharge is yet to stop. Anybody with advice on what I may do next? Thanks and God bless
please if something isn’t right go back and see your surgeon have it taken care of.