Amputation
Definition
Amputation is the surgical removal of a limb or body part. It is performed to remove diseased tissue or relieve pain.
Purpose
Arms, legs, hands, feet, fingers, and toes can all be amputated. In the United States, there are approximately
Here in the United States, the most common causes of amputation of the lower extremity are: disease (70%), trauma (22%), congenital or birth defects (4%), and tumors (4%). As for upper extremity amputation, it is usually performed because of trauma or birth defect. Seldom is disease as great a contributing factor. The causes of amputation differ significantly in various countries. For example, countries with a recent history of warfare and civil unrest will have a higher incidence of amputations, due to war itself or its technology (landmines, uncontrolled ordnance, etc).
Among the diseases and conditions that may lead to amputation of an extremity, the most prevalent are:
- hardening of the arteries
- arterial embolism
- impaired circulation as a complication of diabetes mellitus
- gangrene
- severe frostbite
- Raynaud's disease
- Buerger's disease
More than 90% of amputations performed in the United States are due to circulatory complications of diabetes. Sixty to eighty percent of these operations involve the legs.
Demographics
Most amputations involve small body parts such as a finger, rather than an entire limb. About 65,000 amputations are performed in the United States each year.
In the United States, there are approximately 350,000 amputees, with some 135,000 new amputations occurring each year. The number of amputees worldwide is not currently known.
Description
Amputations can be either planned or emergency procedures. Injury and arterial embolisms are the main reasons for emergency amputations. The operation is performed under regional or general anesthesia by a general or orthopedic surgeon in a hospital operating room .
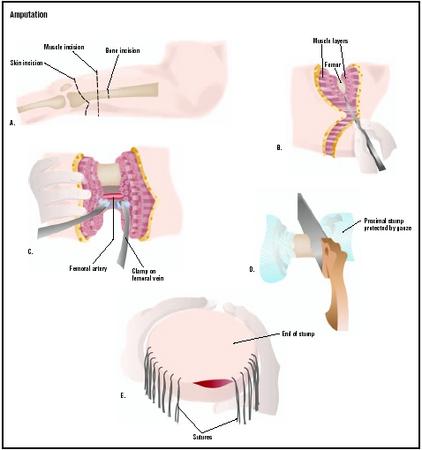
Details of the operation vary slightly depending on what part is to be removed. All amputations consist of a two-fold surgical procedure: to remove diseased tissue so that the wound will heal cleanly, and to construct a stump that will allow the attachment of a prosthesis or artificial replacement part.
The surgeon makes an incision around the part to be amputated. The part is removed, and the bone is smoothed. A flap is constructed of muscle, connective tissue, and skin to cover the raw end of the bone. The flap is closed over the bone with sutures (surgical stitches) that remain in place for about one month. Often, a rigid dressing or cast is applied that stays in place for about two weeks.
Diagnosis/Preparation
Before an amputation is performed, extensive testing is done to determine the proper level of amputation. The goal of the surgeon is to find the place where healing is most likely to be complete, while allowing the maximum amount of limb to remain for effective rehabilitation.
The greater the blood flow through an area, the more likely healing is to occur. These tests are designed to measure blood flow through the limb. Several or all of them can be done to help choose the proper level of amputation.
- measurement of blood pressure in different parts of the limb
- xenon 133 studies, which use a radiopharmaceutical to measure blood flow
- oxygen tension measurements in which an oxygen electrode is used to measure oxygen pressure under the skin (If the pressure is 0, the healing will not occur. If the pressure reads higher than 40mm Hg [40 milliliters of mercury], healing of the area is likely to be satisfactory.)
- laser doppler measurements of the microcirculation of the skin
- skin fluorescent studies that also measure skin microcirculation
- skin perfusion measurements using a blood pressure cuff and photoelectric detector
- infrared measurements of skin temperature
No one test is highly predictive of healing, but taken together, the results give the surgeon an excellent idea of the best place to amputate.
Aftercare
After amputation, medication is prescribed for pain, and patients are treated with antibiotics to discourage infection. The stump is moved often to encourage good circulation. Physical therapy and rehabilitation are started as soon as possible, usually within 48 hours. Studies have shown that there is a positive relationship between early rehabilitation and effective functioning of the stump and prosthesis. Length of stay in the hospital depends on the severity of the amputation and the general health of the amputee, but ranges from several days to two weeks.
Rehabilitation is a long, arduous process, especially for above the knee amputees. Twice daily physical therapy is not uncommon. In addition, psychological counseling is an important part of rehabilitation. Many people feel a sense of loss and grief when they lose a body part. Others are bothered by phantom limb syndrome, where they feel as if the amputated part is still in place. They may even feel pain in this limb that does not exist. Many amputees benefit from joining self-help groups and meeting others who are also living with amputation. Addressing the emotional aspects of amputation often speeds the physical rehabilitation process.
Risks
Amputation is major surgery. All the risks associated with the administration of anesthesia exist, along with the possibility of heavy blood loss and the development of blood clots. Infection is of special concern to amputees. Infection rates in amputations average 15%. If the stump becomes infected, it is necessary to remove the prosthesis and sometimes to amputate a second time at a higher level.
Failure of the stump to heal is another major complication. Nonhealing is usually due to an inadequate blood supply. The rate of nonhealing varies from 5–30% depending on the facility. Centers that specialize in amputation usually have the lowest rates of complication.
Persistent pain in the stump or pain in the phantom limb is experienced by most amputees to some degree. Treatment of phantom limb pain is difficult. One final complication is that many amputees give up on the rehabilitation process and discard their prosthesis. Better fitting prosthetics and earlier rehabilitation have decreased the incidence of this problem.
Normal results
The five year survival rate for all lower extremity amputees is less than 50%. For diabetic amputees, the rate is less than 40%. Up to 50% of people who have one leg amputated because of diabetes will lose the other within five years. Amputees who walk using a prosthesis have a less stable gait. Three to five percent of these people fall and break bones because of this instability. Although the fractures can be treated, about half the amputees who suffer them then remain wheelchair bound.
Alternatives
Alternatives to amputation depend on the medical cause underlying the decision to amputate and the degree of medical urgency. In some cases, drug therapy may be considered as an alternative.
For example, one serious complication of diabetes is the development of foot ulcers that often lead to amputation. Some studies have suggested non-surgical treatment of diabetic foot ulcers with a new, recombinant drug (Becaplermin/Regranex). Combined with competent ulcer nursing, the drug leads to fewer amputations compared to the alternative of ulcer nursing on its own.
Resources
books
Meier, R. H. Functional Restoration of Adults and Children With Upper Extremity Amputation. New York: Demos Medical Publishing, 2003.
Murdoch, G. and A. Bennett Wilson. A Primer on Amputations and Artificial Limbs. Springfield: Charles C. Thomas Pub. Ltd., 1998.
Watts, H. and M. Williams. Who Is Amelia?: Caring for Children With Limb Difference. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1998.
periodicals
Buzato, M. A., E. C. Tribulatto, S. M. Costa, W G. Zorn, and B. van Bellen. "Major amputations of the lower leg. The patients two years later." Acta Chirurgica Belgica 102 (August 2002): 248–252.
Cull, D. L., S. M. Taylor, S. E. Hamontree, E. M. Langan, B. A. Snyder, T. M. Sullivan, and J. R. Youkey. "A reappraisal of a modified through-knee amputation in patients with peripheral vascular disease." American Journal of Surgery 182 (July 2001): 44–48.
Gerstein, H. and D. Hunt. "Foot ulcers and amputations in diabetes." Clinical Evidence 7 (June 2002): 521–528.
Hagberg, K. and R. Branemark. "Consequences of non-vascular trans-femoral amputation: a survey of quality of life, prosthetic use and problems." Prosthetic Orthotherapy International 25 (December 2001): 186–194.
Kazmers, A., A. J. Perkins and L. A. Jacobs. "Major lower extremity amputation in Veterans Affairs medical centers." Annals of Vascular Surgery 14 (May 2000): 216–222.
Oyibo, S. O., E. B. Jude, I. Tarawneh, H. C. Nguyen, D. G. Armstrong, L. B. Harkless, and A. J. Boulton. "The effects of ulcer size and site, patient's age, sex and type and duration of diabetes on the outcome of diabetic foot ulcers." Diabetic Medicine 18 (February 2001): 133–138.
organizations
American Academy of Orthopaedic Surgeons. 6300 North River Road, Rosemont, Illinois 60018-4262. Phone (847) 823-7186. http://www.aaos.org .
American College of Surgeons. 633 N. Saint Clar st., Chicago, IL 60611-3211. (312) 202-5000. http://www.facs.org .
American Diabetes Association. 1701 North Beauregard Street, Alexandria, VA 22311. (800) 342-2383. http://www.diabetes.org .
National Amputation Foundation. 40 Church Street, Malverne, NY 11565. (516) 887-3600. http://www.nationalamputation.org/ .
other
The Amputee Newswire. http://www.amputee-online.com/amputation/ .
Amputation Prevention Global Resource Center Page. http://www.diabetesresource.com .
Cripworld Guide to Amputation. http://www.cripworld.com/amputee/ampinfo.htm .
Tish Davidson, A.M. Monique Laberge, Ph.D.
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Amputations are performed in a hospital, usually by an orthopaedic surgeon. Orthopedics is a medical specialty that focuses on the diagnosis, care and treatment of patients with disorders of the bones, joints, muscles, ligaments, tendons, nerves, and skin. These elements make up the musculoskeletal system. The physicians who specialize in this area are called orthopedic surgeons or orthopedists. Orthopedic surgery is a specialty of immense variety, and includes amputation surgery.
QUESTIONS TO ASK THE DOCTOR
- Is amputation the best solution?
- How long is the procedure?
- How long will it take to recover from the amputation?
- What are the major risks of the surgery?
- What kind of pain will I have after the amputation and for how long?
- What steps will you take to minimize those risks?
- How long will I have to remain in bed?
- When will I be fitted with my first prosthesis?
Thank you very much.
Sincerely,
John
Julia 2147895071 Bless you!
Chester Deaver
817-565-2905
my name is sachin kumar.reason is that behind me,my father age is 45-50 he is not speak and body is so tied and weight is also low... .when he speak after that he not speak properly.so u given me suggest...he is diabetics also...
my mail id=sachin_it8@yahoo.com
My father age of 68 to 70 lost of two above the knee legs due to the sugar is there any solution he need to walk so please help me and if its possible please let me know the cost for the legs