Bronchoscopy
Definition
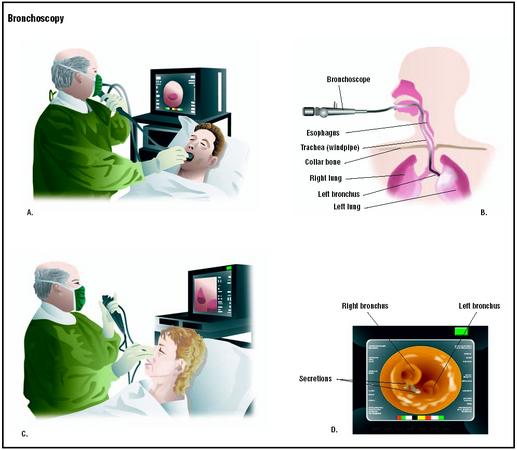
Bronchoscopy is a procedure in which a hollow, flexible tube called a bronchoscope is inserted into the airways through the nose or mouth to provide a view of the tracheobronchial tree. It can also be used to collect bronchial and/or lung secretions and to perform tissue biopsy.
Purpose
During a bronchoscopy, the physician can visually examine the lower airways, including the larynx, trachea, bronchi, and bronchioles. The procedure is used to examine the mucosal surface of the airways for abnormalities that might be associated with a variety of lung diseases. Its use may be diagnostic or therapeutic.
Bronchoscopy may be used to examine and help diagnose:
- diseases of the lung, such as cancer or tuberculosis
- congenital deformity of the lungs
- suspected tumor, obstruction, secretion, bleeding, or foreign body in the airways
- airway abnormalities, such as tracheal stenoses
- persistent cough, or hemoptysis, that includes blood in the sputum
Bronchoscopy may also be used for the following therapeutic purposes:
- to remove a foreign body in the lungs
- to remove excessive secretions
Bronchoscopy can also be used to collect the following biopsy specimens:
- sputum
- tissue samples from the bronchi or bronchioles
- cells collected from washing the lining of the bronchi or bronchioles
If the purpose of the bronchoscopy is to take tissue samples or biopsy, a forceps or bronchial brush are used to obtain cells. Alternatively, if the purpose is to identify an infectious agent, a bronchoalveolar lavage can be performed to gather fluid for culture purposes. If any foreign matter is found in the airways, it can be removed as well.
The instrument used in bronchoscopy, a bronchoscope, is a slender, flexible tube less than 0.5 in (2.5 cm) wide and approximately 2 ft (0.3 m) long that uses fiberoptic technology (very fine filaments that can bend and carry light). There are two types of bronchoscopes, a standard tube that is more rigid and a fiberoptic tube that is more flexible. The rigid instrument does not bend, does not see as far down into the lungs as the flexible one, and may carry a greater risk of causing injury to nearby structures. Because it can cause more discomfort than the flexible bronchoscope, it usually requires general anesthesia. However, it is useful for taking large samples of tissue and for removing foreign bodies from the airways. During the procedure, the airway is never blocked since oxygen can be supplied through the bronchoscope.
Demographics
In 2000, the National Hospital Discharge Survey and the National Survey of Ambulatory Surgery Reports outlined the following rates for bronchoscopy with or without biopsy at short-stay hospitals in the United States:
- Both sexes: 8.9 per 10,000 population
- Males: 10.6 per 10,000 population
- Females: 7.3 per 10,000 population
According to the National Cancer Institute, cancer of the lung and bronchi is the second most common cancer among both men and women and is the leading cause of cancer death in both sexes in the United States. Among men, lung cancer incidence rates per 100,000 people range from a low of approximately 14 among American Indians to a high of 117 among African Americans. Between these two extremes, rates fall into two groups ranging from 42 to 53 for Hispanics, Japanese, Chinese, Filipinos, and Koreans and from 71 to 89 for Vietnamese, Caucasians, Alaska natives, and Hawaiians. The range among women is much narrower, from a rate of about 15 among Japanese to nearly 51 among Alaska Natives, only a three-fold difference. Rates for the remaining female populations fall roughly into two groups with low rates of 16–25 for Korean, Filipino, Hispanic, and Chinese women, and rates of 31–44 among Vietnamese, Caucasian, Hawaiian, and African American women. The rates among men are about two to three times greater than the rates among women in each of the racial/ethnic groups.
Description
Bronchoscopy is usually performed in an endoscopy room, but may also be performed at the bedside. The patient is placed on his back or sits upright. A pulmonologist, a specialist trained to perform the procedure, sprays an anesthetic into the patient's mouth or throat. When anesthesia has taken effect and the area is numb, the bronchoscope is inserted into the patient's mouth and passed into the throat. If the bronchoscope is passed through the nose, an anesthetic jelly is inserted into one nostril. While the bronchoscope is moving down the throat, additional anesthetic is put into the bronchoscope to anesthetize the lower airways. The physician observes the trachea, bronchi, and the mucosal lining of these passageways looking for any abnormalities that may be present. If samples are needed, a bronchial lavage may be performed, meaning that a saline solution is introduced to flush the area prior to collecting cells for laboratory
Preparation
The patient should fast for six to 12 hours prior to the procedure and refrain from drinking any liquids the day of the procedure. Smoking should be avoided for 24 hours prior to the procedure and patients should also avoid taking any aspirin or ibuprofen-type medications. The bronchoscopy itself takes about 45–60 minutes. Prior to the bronchoscopy, several tests are usually done, including a chest x ray and blood work. Sometimes a bronchoscopy is done under general anesthesia, in which case the patient will have an intravenous (IV) line in the arm. More commonly, the procedure is performed under local anesthesia, which is sprayed into the nose or mouth. This is necessary to inhibit the gag reflex. A sedative also may be given. A signed consent form is necessary for this procedure.
Aftercare
After the bronchoscopy, the vital signs (heart rate, blood pressure, and breathing) are monitored. Sometimes patients have an abnormal reaction to anesthesia. Any sputum should be collected in an emesis basin so that it can be examined for the presence of blood. If a biopsy was taken, the patient should not cough or clear the throat as this might dislodge any blood clot that has formed and cause bleeding. No food or drink should be consumed for about two hours after the procedure or until the anesthesia wears off. There is a significant risk for choking if anything (including water) is ingested before the anesthetic wears off, and the gag reflex has returned. To test if the gag reflex has returned, a spoon is placed on the back of the tongue for a few seconds with light pressure. If there is no gagging, the process is repeated after 15 minutes. The gag reflex should return in one to two hours. Ice chips or clear liquids should be taken before the patient attempts to eat solid food.
Patients are informed that after the anesthetic wears off the throat may be irritated for several days.
Patients should notify their health care provider if they develop any of these symptoms:
- hemoptysis (coughing up blood)
- shortness of breath, wheezing, or any trouble breathing
- chest pain
- fever, with or without breathing problems
Risks
Use of the bronchoscope mildly irritates the lining of the airways, resulting in some swelling and inflammation, as well as hoarseness caused from abrading the vocal cords. If this abrasion is more serious, it can lead to respiratory difficulty or bleeding of the lining of the airways.
The bronchoscopy procedure is also associated with a small risk of disordered heart rhythm (arrhythmia), heart attacks, low blood oxygen (hypoxemia), and pneumothorax (a puncture of the lungs that allows air to escape into the space between the lung and the chest wall). These risks are greater with the use of a rigid bronchoscope than with a fiberoptic bronchoscope. If a rigid tube is used, there is also a risk of chipped teeth. The risk of transmitting infectious disease from one patient to another by the bronchoscope is also present. There is also a risk of infection from endoscopes inadequately reprocessed by the automated endoscope reprocessing (AER) system. The Centers for Disease Control (CDC) reported cases of patient-to-patient transmission of infections following bronchoscopic procedures using bronchoscopes that were inadequately reprocessed by AERs. Investigation of the incidents revealed inconsistencies between the reprocessing instructions provided by the manufacturer of the bronchoscope and the manufacturer of the AER; or that the bronchoscopes were inadequately reprocessed.
Normal results
If the results of the bronchoscopy are normal, the windpipe (trachea) appears as smooth muscle with C-shaped rings of cartilage at regular intervals. There are no abnormalities either in the trachea or in the bronchi of the lungs.
Bronchoscopy results may also confirm a suspected diagnosis. This may include swelling, ulceration, or deformity in the bronchial wall, such as inflammation, stenosis, or compression of the trachea, neoplasm, and foreign bodies. The bronchoscopy may also reveal the presence of atypical substances in the trachea and bronchi. If samples are taken, the results could indicate cancer, disease-causing agents, or other lung diseases. Other findings may include constriction or narrowing (stenosis), compression, dilation of vessels, or abnormal branching of the bronchi. Abnormal substances that might be found in the airways include blood, secretions, or mucous plugs.
Morbidity and mortality rates
Bronchoscopy belongs to the group of procedures associated with highest inpatient mortality with a 12.7% mortality rate.
Alternatives
Depending upon the purpose of the bronchoscopy, alternatives may include a chest x ray or a computed tomography (CT) scan. If the purpose is to obtain biopsy specimens, one option is to perform surgery, which carries greater risks. Another option is percutaneous biopsy guided by CT.
Resources
books
Bolliger, C. T., and P. N. Mathur, eds. Interventional Bronchoscopy. (Progress in Respiratory Research, Vol. 30). Basel: S. Karger Publishing, 1999.
Koppen, W., J. F. Turner, and A. C. Mehta, eds. Flexible Bronchoscopy. 2nd ed. Oxford: Blackwell Publishers, 2004.
Loeb, S., ed. Illustrated Guide to Diagnostic Tests. Springhouse, PA: Springhouse Corporation, 1994.
Pagana, Kathleen D., and Timothy J. Pagana. Diagnostic Testing and Nursing Implications. 5th ed. St. Louis: Mosby, 1999.
periodicals
Diette, G. B., N. Lechtzin, E. Haponik, A. Devrotes, and H. R. Rubin. "Distraction Therapy with Nature Sights and Sounds Reduces Pain during Flexible Bronchoscopy: A Complementary Approach to Routine Analgesia." Chest 123 (March 2003): 941–948.
Nakamura, C. T., J. F. Ripka, K. McVeigh, N. Kapoor, and T. G. Keens. "Bronchoscopic Instillation of Surfactant in Acute Respiratory Distress Syndrome." Pediatric Pulmonology 31, no. 4 (April 2001): 317–320.
Starobin, D., G. Fink, D. Shitrit, G. Izbicki, D. Bendayan, I. Bakal, and M. R. Kramer. "The Role of Fiberoptic Bronchoscopy Evaluating Transplant Recipients with Suspected Pulmonary Infections: Analysis of 168 Cases in a Multi-organ Transplantation Center." Transplantation Proceedings 35 (March 2003): 659–660.
Wu, K. H., T. T. Man, K. L. Wong, C. F. Lin, C. C. Chen, and C. R. Cheng. "Bronchoscopy and Anesthesia for Preschool-aged Patients: A Review of 228 Cases." Internal Surgery 87 (October-December 2002): 252–255.
Yang, C. C., and K. S. Lee. "Comparison of Direct Vision and Video Imaging during Bronchoscopy for Pediatric Airway Foreign Bodies." Ear, Nose, and Throat Journal 82 (February 2003): 129–133.
organizations
American College of Chest Physicians. 3300 Dundee Road, Northbrook, IL 60062. (800) 343-2227.
The Association of Perioperative Registered Nurses, Inc. (AORN). 2170 South Parker Rd, Suite 300, Denver, CO 80231-5711. (800) 755-2676. http://www.aorn.org/ .
other
"Bronchoscopy." Medline Plus. [cited April 2003]. http://www.nlm.nih.gov/medlineplus/ency/article/003857.htm .
Public Health Advisory: Infections from Endoscopes Inadequately Reprocessed by an Automated Endoscope Reprocessing System. U. S. Food and Drug Administration, Center for Devices and Radiological Health. September 1999 [cited April 2003]. http://www.fda.gov/cdrh/safety/endoreprocess.html .
Maggie Boleyn, RN, BSN Monique Laberge, Ph D
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
The test is usually performed in a hospital or clinic by a pulmonologist, a physician specializing in diseases of the lungs. Nursing staff assist by providing education, monitoring the patient, and conducting tests, including checking blood pressure, pulse, and respiratory rate prior to the patient's discharge.
QUESTIONS TO ASK THE DOCTOR
- What will happen during the procedure?
- Will it hurt?
- How long will the test last?
- How many bronchoscopies do you perform each year?
- Are there any risks associated with the procedure?
Scott Baker RRT
The reason I had it done was because I was coughing up blood with my speutum.
The results indicated that I had several small white lesions on my right lung.
My provider and surgeon informed me that because I was a heavy smoker in the past, that is why I have those lesions because of past damage to my lung.
He asked if I could make an appointment for a complete CT Scan of the body and then make an appointment for another procedure and most likey he would do another exploritory as before and gather samples of the both lesions to see if they were cancerous or not.
I have heard from others that this might prove dangerous to me if bleeding does occur in the gathering of the leisons and if they are cancerous, could they spread?
I am a 73 white-male; ex-smoker and consumer of alcohol in the past.
I would appreciate any feedback concerning his comments made to me after the procedure. Thank You,
James "Jim" Miller