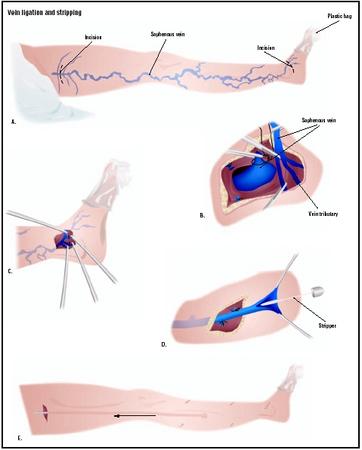
Vein ligation and stripping
Definition
Vein ligation and stripping is a surgical approach to the treatment of varicose veins. It is also sometimes called phlebectomy. Ligation refers to the surgical tying off of a large vein in the leg called the greater saphenous vein, while stripping refers to the removal of this vein through incisions in the groin area or behind the knee. If some of the valves in the saphenous vein are healthy, the weak portion of the vein can be closed off by ligation. If the entire vein is weak, it is closed off and pulled downward and out through an incision made below it. Tying and removal of the greater saphenous vein is done to reduce the pressure of blood flowing backward through this large vein into the smaller veins that feed into it.
Phlebectomy is one of the oldest forms of treatment for varicose veins; the earliest description of it was written by Aulus Cornelius Celsus, a Roman historian of medicine, in A . D . 45. The first description of a phlebectomy hook comes from a textbook on surgery published in 1545. The modern technique of ambulatory (outpatient) phlebectomy was developed around 1956 by a Swiss dermatologist named Robert Muller. As of 2003, surgical ligation and stripping of the saphenous vein is performed less frequently because of the introduction of less invasive forms of treatment.
Purpose
The purpose of vein ligation and stripping is to reduce the number and size of varicose veins that cannot be treated or closed by other measures. The reasons for vascular surgery in general include:
- Improvement of the appearance of the legs. Large varicose veins are considered disfiguring by many people.
- Relief from pain, leg cramps, and fatigue that may be associated with varicose veins.
- Treatment of skin problems that may develop as complications of varicose veins. These include chronic eczema, skin ulceration, external bleeding, and abnormal pigmentation of the skin.
- Prevention of such disorders as thrombophlebitis and pulmonary blood clots.
Demographics
The World Health Organization (WHO) estimates that about 25% of adults around the world have some type of venous disorder in the legs. The proportion of the general population with varicose veins is higher, however, in the developed countries. The American College of Phlebology (ACP), which is a group of dermatologists, plastic surgeons, gynecologists, and general surgeons with special training in the treatment of venous disorders, states that more than 80 million people in the United States suffer from varicose veins. In the past, the female to male ratio has been close to four to one, but this figure is changing due to the rapid rise in obesity among adult males in the past two decades.
Varicose veins are more common in middle-aged and elderly adults than in children or young adults. Although varicose veins tend to run in families, they do not appear to be associated with specific racial or ethnic groups.
Description
Causes of varicose veins
To understand why surgical treatment of varicose veins is sometimes necessary, it is helpful to start with a brief description of the venous system in the human body. The venous part of the circulatory system returns blood to the heart to be pumped to the lungs for oxygenation, in contrast to the arterial system, which carries oxygenated blood away from the heart to be distributed throughout the body. Veins are more likely than arteries to expand or dilate if blood volume or pressure increases, because they consist of only one layer of tissue; this is in contrast to arteries, in which there are three layers.
There are three major categories of veins: superficial veins, deep veins, and perforating veins. All varicose veins are superficial veins; they lie between the skin and a layer of fibrous connective tissue called fascia, which cover and support the muscles and the internal organs. The deep veins of the body lie within the muscle fascia. This distinction helps to explain why a superficial vein can be removed or closed without damage to the deep circulation in the legs. Perforating veins are veins that connect the superficial and deep veins.
Veins contain one-way valves that push blood inward and upward toward the heart against the force of gravity when they are functioning normally. The blood pressure in the superficial veins is usually low, but if it rises and remains at a higher level over a period of time, the valves in the veins begin to fail. The blood flows backward and collects in the lower veins, and the veins dilate, or expand. Veins that are not functioning properly are said to be incompetent. As the veins expand, they become more noticeable under the surface of the skin. Small veins, or capillaries, often appear as spider-shaped or tree-like networks of reddish or purplish lines under the skin. The medical term for these is telangiectasias, but they are commonly known as spider veins or thread veins. Larger veins that form flat, blue-green networks often found behind the knee are called reticular varicosities. True varicose veins are formed when the largest superficial veins become distorted and twisted by a long-term rise in blood pressure in the legs.
The most important veins in the lower leg are the two saphenous veins—the greater saphenous vein, which runs from the foot to the groin area, and the short saphenous vein, which runs from the ankle to the knee. It is thought that varicose veins develop when the valves at the top of the greater saphenous vein fail, allowing more blood to flow backward down the leg and increase the pressure on the valves in the smaller veins in turn. The practice of ligation and stripping of the greater saphenous vein is based on this hypothesis.
Some people are at increased risk for developing varicose veins. These risk factors include:
- Sex. Females in any age group are more likely than males to develop varicose veins. It is thought that female sex hormones contribute to the development of varicose veins by making the veins dilate more easily. Many women experience increased discomfort from varicose veins during their menstrual periods.
- Genetic factors. Some people have veins with abnormally weak walls or valves. They may develop varicose veins even without a rise in blood pressure in the superficial veins. This characteristic tends to run in families.
- Pregnancy. A woman's total blood volume increases during pregnancy, which increases the blood pressure in the venous system. In addition, the hormonal changes of pregnancy cause the walls and valves in the veins to soften.
- Using birth control pills.
- Obesity. Excess body weight increases the pressure on the veins.
- Occupational factors. People who have jobs that require standing or sitting for long periods of time—without the opportunity to walk or move around—are more likely to develop varicose veins.
Ambulatory phlebectomy
Ambulatory phlebectomy is the most common surgical procedure for treating medium-sized varicose veins, as of early 2003. It is also known as stab avulsion or micro-extraction phlebectomy. An ambulatory phlebectomy is performed under local anesthesia. After the patient's leg has been anesthetized, the surgeon makes a series of very small vertical incisions 1–3 mm in length along the length of the affected vein. These incisions do not require stitches or tape closure afterward. Beginning with the more heavily involved areas of the leg, the surgeon inserts a phlebectomy hook through each micro-incision. The vein segment is drawn through the incision, held with a mosquito clamp, and pulled out through the incision. This technique requires the surgeon to be especially careful when removing varicose veins in the ankle, foot, or back of the knee.
After all the vein segments have been removed, the surgeon washes the patient's leg with hydrogen peroxide and covers the area with a foam wrap, several layers of cotton wrap, and an adhesive bandage. A compression stocking is then drawn up over the wrapping. The bandages are removed three to seven days after surgery, but the compression stocking must be worn for another two to four weeks to minimize bruising and swelling. The patient is encouraged to walk around for 10–15 minutes before leaving the office; this mild activity helps to minimize the risk of a blood clot forming in the deep veins of the leg.
Transilluminated powered phlebectomy
Transilluminated powered phlebectomy (TIPP) is a newer technique that avoids the drawbacks of stab avulsion phlebectomy, which include long operating times, the risk of scar formation, and a relatively high risk of infection developing in the micro-incisions. Transilluminated powered phlebectomy performed with an illuminator and a motorized resector. After the patient has been anesthetized with light general anesthesia, the surgeon makes only two small incisions: one for the illuminating device and the other for the resector. After making the first incision and introducing the illuminator, the surgeon uses a technique called tumescent anesthesia to plump up the tissues around the veins and make the veins easier to remove. Tumescent anesthesia was originally developed for liposuction . It involves the injection of large quantities of a dilute anesthetic into the tissues surrounding the veins until they become firm and swollen.
After the tumescent anesthesia has been completed, the surgeon makes a second incision to insert the resector, which draws the vein by suction toward an inner blade. The suction then removes the tiny pieces of venous tissue left by the blade. After all the clusters of varicose veins have been treated, the surgeon closes the two small incisions with a single stitch or Steri-Strips. The incisions are covered with a gauze dressing and the leg is wrapped in a sterile compression dressing.
Diagnosis/Preparation
Diagnosis
Vein ligation and stripping and ambulatory phlebectomies are considered elective procedures; they are not performed on an emergency basis. The process of diagnosis may begin with the patient's complaints about the appearance of the legs or of pain and cramps, as well as with the physician's observations. It is important to note that there is no correlation between the size or number of a patient's varicose veins and the amount of pain that is experienced. Some people have experience considerable discomfort from fairly small varices, while others may have no symptoms from clusters of extremely swollen varicose veins. If the patient mentions pain, burning sensations, or other physical symptoms, the doctor will need to rule out other possible causes, such as nerve root irritation, osteoarthritis, diabetic neuropathy, or problems in the arterial circulation. Relief of pain when the leg is elevated is the most significant diagnostic sign of varicose veins.
After taking the patient's medical history and a family history of venous disorders, the doctor examines the patient from the waist down to note the location of varicose veins and to palpate (touch with gentle pressure) for signs of other venous disorders. Palpation helps the doctor locate both normal and abnormal veins; further, some varicose veins can be detected by touch even though they cannot be seen through the skin. Ideally, the examiner will have a small raised platform for the patient to stand on during the physical examination . The doctor will ask the patient to turn slowly while standing, and will be looking for scars or other signs of trauma, bulges and areas of discoloration in the skin, or other indications of chronic venous insufficiency. While palpating the legs, the doctor will note areas of unusual warmth or soreness, cysts, and edema (swelling of the soft tissues due to fluid retention). Next, the doctor will percuss certain parts of the legs where the larger veins lie closer to the surface. By gently tapping or thumping on the skin over these areas, the doctor can feel if there are any fluid waves in the veins and determine whether further testing for venous insufficiency is required.
The next stage of the diagnostic examination is an evaluation of the valves in the patient's greater saphenous vein. The doctor places a tourniquet around the patient's upper thigh while the patient is lying on the examination table with the leg raised. The patient is then asked to stand on the floor. If the valves in this vein are working properly, the lower superficial veins should not fill up rapidly as long as the tourniquet remains tied. This test is known as Trendelenburg's test. It has, however, been largely replaced by the use of duplex Doppler ultrasound—which maps the location of the varicose veins in the patient's leg and provides information about the condition of the valves in the veins. Most insurance companies now also require a Doppler test before authorizing surgical treatment. The doctor's findings will determine whether the greater saphenous vein will require ligation and stripping or endovenous ablation before smaller varicose veins can be treated.
Some disorders or conditions are contraindications for vascular surgery. They include:
- Cellulitis and other infectious diseases of the skin.
- Severe edema associated with heart or kidney disease. These disorders should be brought under control before a phlebectomy is performed.
- Uncontrolled diabetes.
- Disorders that affect the immune system, including HIV infection.
- Severe heart or lung disorders.
Preparation
Patients preparing for vascular surgery are asked to discontinue aspirin or aspirin-related products for a week before the procedure. They should not eat or drink after midnight on the day of surgery. They should not apply any moisturizers, creams, tanning lotions, or sun-block to the legs on the day of the procedure.
A patient scheduled for an ambulatory phlebectomy should arrive at the surgical center about an hour and a half before the procedure. All clothing must be removed before changing into a hospital gown. The patient is asked to walk up and down in the room or hallway for about 20 minutes to make the veins stand out. The surgeon marks the outlines of the veins with an indelible ink marker on the patient's legs while he or she is standing up. An ultrasound may be done at this point to verify the location and condition of the veins. The patient is then taken into the operating room for surgery.
Although patients are encouraged to walk around for a few minutes after an ambulatory phlebectomy, they should make arrangements for a friend or relative to drive them home from the surgical facility.
Aftercare
Surgical ligation and stripping of the greater saphenous vein usually requires an overnight stay in the hospital and two to eight weeks of recovery at home afterward.
Aftercare following surgical treatment of varicose veins includes wearing medical compression stockings that apply either 20–30 mmHg or 30–40 mmHg of pressure for two to six weeks after the procedure. Wearing compression stockings minimizes the risk of edema, discoloration, and pain. Fashion support stockings are a less acceptable alternative because they do not apply enough pressure to the legs.
The elastic surgical dressing applied at the end of an ambulatory phlebectomy should be left in place after returning home. Mild pain-killing medications may be taken for discomfort.
The patient is advised to watch for redness, swelling, pus, fever, and other signs of infection.
Patients are encouraged to walk, ride a bicycle, or participate in other low-impact forms of exercise (such as yoga, and tai chi) to prevent the formation of blood clots in the deep veins of the legs. They should lie down with the legs elevated above heart level for 15 minutes at least twice a day, and use a foot stool when sitting to keep the legs raised.
Risks
Vein ligation and stripping carries the same risks as other surgical procedures under general anesthesia, such as bleeding, infection of the incision, and an adverse reaction to the anesthetic. Patients with leg ulcers or fungal infections of the foot are at increased risk of developing infections in the incisions following surgical treatment of varicose veins.
Specific risks associated with vascular surgery include:
- Deep venous thrombosis.
- Bruising. Bruising is the most common complication of phlebectomies, but heals itself in a few days or weeks.
- Scar formation. Phlebectomy has been found to produce permanent leg scars more frequently than sclerotherapy.
- Injury to the saphenous nerve. This complication results in numbness, tingling, or burning sensations in the area around the ankle. It usually goes away without further treatment within six to 12 months.
- Seromas. A seroma is a collection of uninfected blood serum or lymphatic fluid in the tissues. Seromas usually resolve without further treatment, but can be drained by the surgeon, if necessary.
- Injury to the arteries in the thigh and groin area. This complication is extremely rare, but it can have serious consequences. One example is amputation of the leg.
- Leg swelling. This complication is caused by disruption of the lymphatic system during surgery. This lasts about two to three weeks and can be managed by wearing compression stockings.
- Recurrence of smaller varicose veins.
Normal results
Normal results of vein ligation and stripping, or ambulatory phlebectomy, include reduction in the size and number of varicose veins in the leg. About 95% of patients also experience significant relief of pain.
Morbidity and mortality rates
The mortality rate following vein ligation and stripping has been reported to be one in 30,000. The incidence of deep venous thrombosis (DVT) following vascular surgery is estimated to be 0.6%
Alternatives
Conservative treatments
Patients who are experiencing discomfort from varicose veins may be helped by any or several of the following approaches:
- Exercise. Walking or other forms of exercise that activate the muscles in the lower legs can relieve aching and cramping because these muscles keep the blood moving through the leg veins. One specific exercise that is often recommended is repeated flexing of the ankle joint. Flexing the ankles five to 10 times every few minutes and walking around for one to two minutes every half hour throughout the day helps to prevent the venous congestion that results from sitting or standing in one position for hours at a time.
- Avoiding high-heeled shoes. Shoes with high heels do not allow the ankle to flex fully when the patient is walking. This limitation of the range of motion of the ankle joint makes it more difficult for the leg muscles to contract and force venous blood upwards toward the heart.
- Elevating the legs for 15–30 minutes once or twice a day. This change of position is frequently recommended for reducing edema of the feet and ankles.
- Wearing compression hosiery. Compression benefits the leg veins by reducing inflammation as well as improving venous outflow. Most manufacturers of medical compression stockings now sell some relatively sheer hosiery that looks attractive in addition to providing support.
- Medications. Drugs that have been used to treat the discomfort associated with varicose veins include nonsteroidal anti-inflammatory drugs (NSAIDs) and preparations of vitamins C and E. One prescription medication that is sometimes given to treat circulatory problems in the legs and feet is pentoxifylline, which improves blood flow in the smaller capillaries. Pentoxifylline is sold under the brand name Trendar®.
If appearance is the patient's primary concern, varicose veins can be partially covered with specially formulated cosmetics that come in a wide variety of skin tones. Some of these preparations are available in waterproof formulations for use during swimming and other athletic activities.
Endovenous ablation
Endovenous ablation refers to two newer and less invasive methods for treating incompetent saphenous veins. In the Closure(R) method, which was approved by the Food and Drug Administration (FDA) in 1999, the surgeon passes a catheter into the lumen of the saphenous vein. The catheter is connected to a radiofrequency generator and delivers heat energy to the vein through an electrode in its tip. As the tissues in the wall of the vein are heated, they shrink and coagulate, closing and sealing the vein. Radiofrequency ablation of the saphenous vein has been demonstrated to be safe and at least as effective as surgical stripping of the vein; in addition, patients can return to work the next day. Its chief risk is loss of feeling in a patch of skin about the size of a quarter above the knee. This numbness usually resolves in about six months.
Endovenous laser treatment, or EVLT, uses a laser instead of a catheter with an electrode to heat the tissues in the wall of an incompetent vein in order to close the vein. Although EVLT appears to be as safe and effective as radiofrequency ablation, patients experience more discomfort and bruising afterward; most require two to three days of recovery at home after laser treatment.
Sclerotherapy
Sclerotherapy is a treatment method in which irritating chemicals in liquid or foam form are injected into spider veins or smaller reticular varicosities to close them off. The chemicals cause the vein to become inflamed, and leads to the formation of fibrous tissue and closing of the lumen, or central channel of the vein. Sclerotherapy is sometimes used in combination with other techniques to treat larger varicose veins.
Complementary and alternative (CAM) treatments
According to Dr. Kenneth Pelletier, former director of the program in complementary and alternative treatments at Stanford University School of Medicine, horse chestnut extract works as well as compression stockings when used as a conservative treatment for varicose veins. Horse chestnut ( Aesculus hippocastanum ) preparations have been used in Europe for some years to treat circulatory problems in the legs; most recent research has been carried out in Great Britain and Germany. The usual dosage is 75 mg twice a day, at meals. The most common side effect of oral preparations of horse chestnut is occasional indigestion in some patients.
See also Sclerotherapy for varicose veins .
Resources
books
Pelletier, Kenneth R., M.D. The Best Alternative Medicine , Part II, "CAM Therapies for Specific Conditions: Varicose Veins." New York: Simon & Schuster, 2002.
"Varicose Veins." Section 16, Chapter 212 in The Merck Manual of Diagnosis and Therapy , edited by Mark H. Beers, M.D., and Robert Berkow, M.D. Whitehouse Station, NJ: Merck Research Laboratories, 1999.
periodicals
Bergan, J. J., N. H. Kumins, E. L. Owens, and S. R. Sparks. "Surgical and Endovascular Treatment of Lower Extremity Venous Insufficiency." Journal of Vascular and Interventional Radiology 13 (June 2002): 563-568.
Brethauer, S. A., J. D. Murray, D. G. Hatter, et al. "Treatment of Varicose Veins: Proximal Saphenofemoral Ligation Comparing Adjunctive Varicose Phlebectomy with Sclerotherapy at a Military Medical Center." Vascular Surgery 35 (January-February 2001): 51-58.
de Roos, K. P., F. H. Nieman, and H. A. Neumann. "Ambulatory Phlebectomy Versus Compression Sclerotherapy: Results of a Randomized Controlled Trial." Dermatologic Surgery 29 (March 2003): 221-226.
Feied, Craig, M.D., Robert Weiss, M.D., and Robert B. Hashemiyoon, M.D. "Varicose Veins and Spider Veins." eMedicine , November 20, 2001 [cited April 10, 2003]. http://www.emedicine.com/derm/topic475.htm .
MacKay, D. "Hemorrhoids and Varicose Veins: A Review of Treatment Options." Alternative Medicine Review 6 (April 2001): 126-140.
Min, R. J., S. E. Zimmet, M. N. Isaacs, and M. D. Forrestal. "Endovenous Laser Treatment of the Incompetent Greater Saphenous Vein." Journal of Vascular and Interventional Radiology 12 (October 2001): 1167-1171.
Pittler, M. H., and E. Ernst. "Horse-Chestnut Seed Extract for Chronic Venous Insufficiency. A Criteria-Based Systematic Review." Archives of Dermatology 134 (November 1998): 1356-1360.
Proebstle, T. M., D. Gul, A. Kargl, and J. Knop. "Endovenous Laser Treatment of the Lesser Saphenous Vein with a 940-nm Diode Laser: Early Results." Dermatologic Surgery 29 (April 2003): 357-361.
Ramelet, A. A. "Phlebectomy. Technique, Indications and Complications." International Angiology 21 (June 2002): 46-51.
Weiss, Robert, and Albert-Adrien Ramelet. "Varicose Veins Treated with Ambulatory Phlebectomy." eMedicine , May 29, 2002 [cited April 13, 2003]. http://www.emedicine.com/derm/topic748.htm .
Zotto, Lisa M., RN. "Treating Varicose Veins with Transilluminated Powered Phlebectomy." AORN Journal 76 (December 2002): 981-990.
organizations
American Academy of Dermatology. 930 East Woodfield Rd., PO Box 4014, Schaumburg, IL 60168. (847) 330-0230. http://www.aad.org .
American Association for Vascular Surgery (AAVS). 900 Cummings Center, #221-U, Beverly, MA 01915. http://www.aavs.vascularweb.org .
American College of Phlebology. 100 Webster Street, Suite 101, Oakland, CA 94607-3724. (510) 834-6500. http://www.phlebology.org .
Peripheral Vascular Surgery Society (PVSS). 824 Munras Avenue, Suite C, Monterey, CA 93940. (831) 373-0508. http://www.pvss.org .
other
Bergan, John J., M.D. Surgery of Varicose Veins . [cited April 13, 2003] http://www.phlebology.org/surgery.html .
Feied, Craig, M.D. Venous Anatomy and Physiology . [cited April 10, 2003] http://www.phlebology.org/syllabus1.htm .
Fronek, Helane S., M.D. Conservative Therapy for Venous Disease . [cited April 10, 2003] http://www.phlebology.org/syllabus4.htm .
Fronek, Helane S., M.D. Functional Testing for Venous Disease . [cited April 10, 2003] http://www.phlebology.org/syllabus3.htm .
Marley, Wayne, M.D. Physical Examination of the Phlebology Patient . [cited April 10, 2003] http://www.phlebology.org/syllabus2.htm .
Olivencia, José A., M.D. Ambulatory Phlebectomy . [cited April 13, 2003] http://www.phlebology.org/amphlebec.html .
Weiss, Robert, M.D. Radiofrequency Endovenous Occlusion (Closure(R) Technique) . [cited April 13, 2003] http://www.phlebology.org/closure.htm .
Rebecca Frey, Ph.D.
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Surgical treatment of varicose veins is usually performed by general surgeons or by vascular surgeons, who are trained in the diagnosis and medical management of venous disorders as well as surgical treatment of them. Most vascular surgeons have completed five years of residency training in surgery after medical school, followed by one to two years of specialized fellowship training.
Phlebectomies and endovenous ablation treatments are performed in ambulatory surgery centers as outpatient procedures. Ligation and stripping of the greater saphenous vein, however, is more commonly performed in a hospital as an inpatient operation.
QUESTIONS TO ASK THE DOCTOR
- Can my varicose veins be treated without ligation and stripping?
- Am I a candidate for treatment with EVLT or radiofrequency ablation?
- What specific technique(s) do you perform most frequently?
- Which treatment technique(s) do you recommend and why?
My left knee joint is in constant pain where the vein was taken out and interferes severly with my sleep as the pain is unbearable at night.I have tried pillows and other things between my knees to separate the to stop the pressure.
Has anyone else got these symptoms ??
It cant be that bad if all doctors recommend patients with varicose veins to get it done
Your comments aren't fair on people waiting to get the procedure done and you're making patients pre surgery anxious
If you've nothing good/ nice to say refrain from saying it please and thank you
I only have one large vein left in each leg according to an ultrasound of my legs. Doctors think it is nerve pain, and I think it is from the surgery, but they call it idiopathic.
. What can I do for this problem? At this time I just take pain medicines. Please give me some good advice.