Vagotomy
Definition
Vagotomy is the surgical cutting of the vagus nerve to reduce acid secretion in the stomach.
Purpose
The vagus nerve trunk splits into branches that go to different parts of the stomach. Stimulation from these branches causes the stomach to produce acid. Too much stomach acid leads to ulcers that may eventually bleed and create an emergency situation.
A vagotomy is performed when acid production in the stomach can not be reduced by other means. The purpose of the procedure is to disable the acid-producing capacity of the stomach. It is used when ulcers in the stomach and duodenum do not respond to medication and changes in diet. It is an appropriate surgery when there are ulcer complications, such as obstruction of digestive flow, bleeding, or perforation. The frequency with which elective vagotomy is performed has decreased in the past 20 years as it has become clear that the primary cause of ulcers is an infection by a bacterium called Helicobacter pylori. Drugs have become increasingly effective in treating ulcers. However, the number of vagotomies performed in emergency situations has remained about the same.
A vagotomy procedure is often performed in conjunction with another gastrointestinal surgery, such as partial removal of the stomach ( antrectomy or subtotal gastrectomy ).
Demographics
Gastric (peptic) ulcers are included under the general heading of gastrointestinal (GI) diseases. GI disorders affect an estimated 25–30% of the world's population. In the United States, 60 million adults experience gastrointestinal reflux at least once a month, and 25 million adults suffer daily from heartburn. Left untreated, these conditions often evolve into ulcers. Four million people have active peptic ulcers; about 350,000 new cases are diagnosed each year. Four times as many duodenal ulcers as gastric ulcers are diagnosed. The first-degree relatives of patients with duodenal ulcer have a two to three times greater risk of developing duodenal ulcer. Relatives of gastric ulcer patients have a similarly increased risk of developing a gastric ulcer.
Description
A vagotomy can be performed using closed (laparoscopic) or open surgical technique. The indications for a laparoscopic vagotomy are the same as open vagotomy.
There are four basic types of vagotomy procedures:
- Truncal or total abdominal vagotomy. The main vagal trunks are divided, and surgery is accompanied by a drainage procedure, such as pyloroplasty .
- Selective (total gastric) vagotomy. The main vagal trunks are dissected to the point where the branch leading to the biliary tree divides, and there is a cut at the section of vagus close to the hepatic branch. This procedure is rarely indicated or performed.
-
Highly selective vagotomy (HSV). HSV selectively deprives the parietal
cells of vagal nerves, and reduces
their sensitivity to stimulation and the release of acid. It does not require a drainage procedure. The branches of Latarjet's nerve are divided from the esophagogastric junction to the crow's foot along the lesser curvature of the stomach.
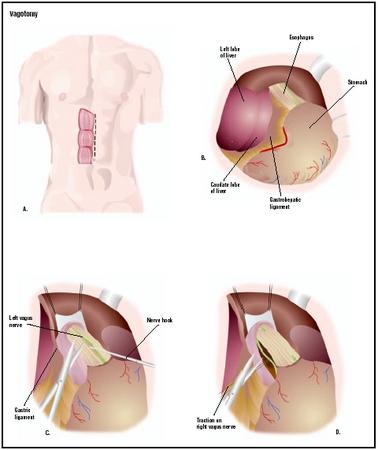 To perform a vagotomy, the surgeon makes an incision in the patient's abdomen (A). The stomach is located (B), and the vagus nerves are cut in turn (C and D). (Illustration by GGS Inc.)
To perform a vagotomy, the surgeon makes an incision in the patient's abdomen (A). The stomach is located (B), and the vagus nerves are cut in turn (C and D). (Illustration by GGS Inc.) - Thoracoscopic vagotomy. Performed through the third, sixth, and seventh left intercostal spaces, the posterior vagus trunk is isolated, clipped, and a segment excised.
A vagotomy is performed under general anesthesia. The surgeon makes an incision in the abdomen and locates the vagus nerve. Either the trunk or the branches leading to the stomach are cut. The abdominal muscles are sewn back together, and the skin is closed with sutures.
Often, other gastrointestinal surgery is performed (e.g., part of the stomach may be removed) at the same time. Vagotomy causes a decrease in peristalsis, and a change in the emptying patterns of the stomach. To ease this, a pyloroplasty is often performed to widen the outlet from the stomach to the small intestine.
Diagnosis/Preparation
A gastroscopy and x rays of the gastrointestinal system determine the position and condition of the ulcer. Standard preoperative blood and urine tests are done. The patient discusses with the anesthesiologist any medications or conditions that might affect the administration of anesthesia.
Aftercare
Patients who have had a vagotomy stay in the hospital for about seven days. Nasogastric suctioning is required for the first three or four days. A tube is inserted through the nose and into the stomach. The stomach contents are then suctioned out. Patients eat a clear liquid diet until the gastrointestinal tract regains function. When patients return to a regular diet, spicy and acidic foods should be avoided.
It takes about six weeks to fully recover from the surgery. The sutures that close the skin can be removed in seven to 10 days. Patients are encouraged to move around soon after the operation to prevent the formation of deep vein blood clots. Pain medication, stool softeners, and antibiotics may be prescribed following the operation.
Risks
Standard surgical risks, such as excessive bleeding and infection, are potential complications. In addition, the emptying patterns of the stomach are changed. This can lead to dumping syndrome and diarrhea. Dumping syndrome is a condition in which the patient experiences palpitations, sweating, nausea, cramps, vomiting, and diarrhea shortly after eating.
The following complications are also associated with vagotomy surgery:
- Gastric or esophageal perforation. May occur from an electrocautery injury or by clipping the branch of the nerve of Latarjet.
- Delayed gastric emptying. Most common after truncal and selective vagotomy, particularly if a drainage procedure is not performed.
People who use alcohol excessively, smoke, are obese, and are very young or very old are at higher risk for complications.
Normal results
Normal recovery is expected for most patients. Ulcers recur in about 10% of those who have vagotomy without stomach removal. Recurrent ulcers are also found in 2–3% of patients who have some portion of their stomach removed.
Morbidity and mortality rates
In the United States, approximately 3,000 deaths per year are due to duodenal ulcer and 3,000 to gastric ulcer. There has been a marked decrease in reported hospitalization and mortality rates for gastric ulcer.
Alternatives
The preferred short-term treatment for gastric ulcers is drug therapy. A recent review surveying medical articles published from 1977 to 1994 concluded that drugs such as cimetidine, ranitidine, famotidine, H2 blockers, and sucralfate were efficient, with omeprazole considered the "gold standard" for active gastric ulcer treatment. Surgical intervention, however, is recommended for people who do not respond to medical therapy.
Resources
books
Ansolon, K. B. Developmental Technology of Gastrectomy & Vagotomy. Rockville, MD: Kabel Publishers, 1995.
Kral, J. Vagal Nerve Function. New York: Elsevier Science Ltd., 1984.
"Stomach and Duodenum." In Current Surgical Diagnosis and Treatment, 10th ed. Edited by Lawrence W. Day. Stamford: Appleton & Lange, 1994.
periodicals
Chang, T. M., D.C. Chan, Y.C. Liu, S.S. Tsou, and T. H. Chen. "Long-term Results of Duodenectomy with Highly Selective Vagotomy in the Treatment of Complicated Duodenal Ulcers." American Journal of Surgery 181 (April 2001): 372-6.
Gilliam, A. D., W.J. Speake, and D. N. Lobo. "Current Practice of Emergency Vagotomy and Helicobacter Pylori Eradication for Complicated Peptic Ulcer in the United Kingdom." British Journal of Surgery 90 (January 2003): 88-90.
Saindon, C. S., F. Blecha, T.I. Musch, D.A. Morgan, R.J. Fels, and M. J. Kenney. "Effect of Cervical Vagotomy on Sympathetic Nerve Responses to Peripheral Interleukin-1beta." Autonomic Neuroscience 87 (March 2001): 243-8.
organizations
American College of Surgeons. 633 N. Saint Clair St., Chicago, IL 60611. (312) 202-5000. http://www.faacs.org .
Society of American Gastrointestinal Endoscopic Surgeons. 2716 Ocean Park Boulevard, Suite 3000, Santa Monica, CA 90405. (310) 314-2404. http://www.sages.org .
Tish Davidson, A.M. Monique Laberge, Ph.D.
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Patients who receive vagotomies are most often seen in emergency situations where bleeding and perforated ulcers require immediate intervention. A vagotomy is usually performed by a board-certified surgeon, either a general surgeon who specializes in gastrointestinal surgery or a gastrointestinal endoscopic surgeon. The procedure is performed in a hospital setting.
QUESTIONS TO ASK THE DOCTOR
- What are the possible complications involved in vagotomy surgery?
- What surgical preparation is needed?
- What type of anesthesia will be used?
- How is the surgery performed?
- How long is the hospitalization?
- How many vagotomies does the surgeon perform in a year?
I have had two scopes done in the last 9 months. I deal with so much pain
everyday! I can't eat spicy food, period or for that matter I can barley eat anything
without getting acid. For example, I ate one slice of bread and got the worst
acid ever. I have really bad acid reflux, but nothing will help it. I have tried everything!
I have been trying to do research on Ulcers, Helicobacter Pylori, and Acid Reflux
but nothing I find matches up and really doesn't make since to me, If anyone knows more about
this and can help me understand it I would really appreciate it! =)
IS THERE A REVERSAL to VAGOTOMY? WOULD A Gastroenterostomy CLOSURE help me? My stomach no longer can digest any food. It's like I have no acid and the food dumps directly into the small intestines.
the symptoms start like this: I start belching a bad tasting and smelling gas that rapidly increases in intensity. Pain in the gut starts and gets more severe, to the point of doubling over. The palms of my hands turn bright red and hives start from there and spread all over. I get very itchy. My blood pressure dramatically increases. I get nausea, sometimes I start vomiting. I end up in the emergency room and they give me a steroid shot that settles it down, sometimes right away, sometimes it takes 15-30 minutes.
My last visit to a gastroenterologist was hopeful in that he gave me a prescription for Levsin. He said that the next time the symptoms start take one of those pills under the tongue and the symptoms will back off.
Well a month ago the symptoms started so I took the pill, but the symptoms kept coming on, so after looking on line for dosage recommendations I took 2 more pills about 2.25 hours later (.125 MG per pill) but the symptoms seem to speed up and I had more pain than ever. The hospital gave me a steroid shot and it settled down.
Here's the thing. I need something to stop those symptoms in their tracks. This summer I'm going to Mexico on a mission trip and I'm scared that it could happen down there and I'd end up dead.
Please help.
The HSV worked. I was in Army Special Forces and I continued to serve in that capacity for another 12 years. For about 10 years I had NO gastric pain at all. I was able to eat foods like pizza, hot dogs, and spaghetti without the heartburn I had experienced all my life. I did have an occasional bout of dumping syndrome that made me woozy for about 20 minutes but that was almost always caused by eating too much starchy food.
After many years an occasional heartburn has returned. It is associated with eating the same foods that used to give me trouble. I take tums when it happens and the burn goes away. These days I must sleep with my head elevated or I get gastric reflux. The bouts of dumping syndrome are very rare.
Much of the success of the HSV has worn off in later years and now, at 57, I am starting to experience what feels like the start of my problems when I was 17. But the HSV allowed me to continue in my high risk profession without any significant side-effects. It allowed me to enjoy a nearly trouble free life for over twenty years. I traveled many places in many countries and made many forays into the wilderness. It wasn't all work. I took my family on several overseas trips, and some of the wilderness trips were for camping, hiking, or hunting. The HSV wasn't painless and it left a big scar but it was well worth it. I am glad I had it done.
i have not had any side effects or ,any sign of ulcers since...it changed my life...maybe i was lucky
my son had the same thing but it had been discovered ( by a perth doctor (aus)) that it was caused by bacteria helicopacter pyloris and just now takes medication.
hope this is useful!
al
i`m a fit healthy 72 yrs old!
my son had the same thing but it had been discovered ( by a perth doctor (aus)) that it was caused by bacteria helicopacter pyloris and just now takes medication.
hope this is useful!
al
i`m a fit healthy 72 yrs old!
I have tried to reply to your question but it keeps telling me no bad language or the code is wrong.
I'd like to know what I'm doing wrong?
Linda don't do the operation, hope I am not too late warning you. GOD Bless, Derek
Now 30 years later I'm having more gastric reflux and have had to stop the omeprazole for 1 week so a 24 hours acid test can check my acid production and oesophagal sphincter operation. Within 36 hours my dumping has returned and I'm dreading the next 6 days before the procedure.
However better to have had the vegotomy as I would have died had I not had it and the partial gastrectomy, and thank heavens for omeprazole!
I wish you all well and hope you find solutions to your particular problems.
I am suffering form Nissen fundo with accidentel injury! PP test came out al compared total vagotomy!!
Fighting this for 3 ,5 years now!! So tired off this!! Please is ther anyone who can offer help maby undo the Nissen..
Desperate..
mariette
I did and do occasionally have the Dumping, and I sometimes need B12. I am now on Nexium, and occasionally Carafate.
Anyone considering having a vagotomy, think twice and gather all of your facts before hand. Be aware, it is not something that will cure everything and will probably create other problems.
Good luck everyone. Jenny