Sclerotherapy for varicose veins
Definition
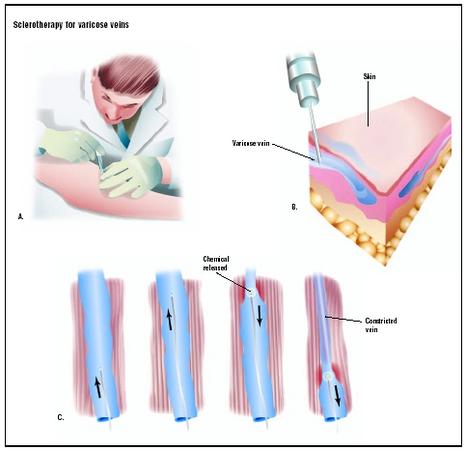
Sclerotherapy, which takes its name from a Greek word meaning "hardening," is a method of treating enlarged veins by injecting an irritating chemical called a sclerosing agent into the vein. The chemical causes the vein to become inflamed, which leads to the formation of fibrous tissue and closing of the lumen, or central channel of the vein.
Purpose
Sclerotherapy in the legs is performed for several reasons. It is most often done to improve the appearance of the legs, and is accomplished by closing down spider veins—small veins in the legs that have dilated under increased venous blood pressure. A spider vein is one type of telangiectasia, which is the medical term for a reddish-colored lesion produced by the permanent enlargement of the capillaries and other small blood vessels. The word telangiectasia comes from three Greek words that mean "end," "blood vessel," and "stretch out." In a spider vein, also called a "sunburst varicosity" there is a central reddish area that is visible to the eye because it lies close to the surface of the skin; smaller veins spread outward from it in the shape of a spider's legs. Spider veins may also appear in two other common patterns—they may look like tiny tree branches or like extra-fine separate lines.
In addition to the cosmetic purposes sclerotherapy serves, it is also performed to treat the soreness, aching, muscle fatigue, and leg cramps that often accompany small- or middle-sized varicose veins in the legs. It is not, however, used by itself to treat large varicose veins.
Because sclerotherapy is usually considered a cosmetic procedure, it is usually not covered by health insurance. People who are being treated for cramps and discomfort in their legs, however, should ask their insurance companies whether they are covered for sclerotherapy. In 2001, the average cost of the procedure was $227.
Sclerotherapy as a general treatment modality is also performed to treat hemorrhoids (swollen veins) in the esophagus.
Demographics
The American College of Phlebology (ACP), a group of dermatologists, plastic surgeons, gynecologists, and general surgeons with special training in the treatment of venous disorders, comments that more than 80 million people in the United States suffer from spider veins or varicose veins. The American Society of Plastic Surgeons (ASPS) estimates that 50% of women over 21 in the United States have spider veins.
Women are more likely to develop spider veins than men, but the incidence among both sexes increases with age. The results of a recent survey of middle-aged and elderly people in San Diego, California, show that 80% of the women and 50% of the men had spider veins. Men are less likely to seek treatment for spider veins for cosmetic reasons, however, because the discoloration caused by spider veins is often covered by leg hair. On the other hand, men who are bothered by aching, burning sensations or leg cramps, can benefit from sclerotherapy.
According to the ASPS, there were 616,879 sclerotherapy procedures performed in the United States in 2001; 97% were performed on women and 3% were done on men. Most people who are treated with sclerotherapy are between the ages of 30 and 60.
Spider veins are most noticeable and common in Caucasians. Hispanics are less likely than Caucasians but more likely than either African or Asian Americans to develop spider veins.
Description
Causes of spider veins
To understand how sclerotherapy works, it is helpful to begin with a brief description of the venous system in the human body. The venous part of the circulatory system returns blood to the heart to be pumped to the lungs for oxygenation. This is in contrast to the arterial system, which carries oxygenated blood away from the heart to be distributed throughout the body. The smallest parts of the venous system are the capillaries, which feed into larger superficial veins. All superficial veins lie between the skin and a layer of fibrous connective tissue called fascia, which covers and supports the muscles and the internal organs. The deeper veins of the body lie within the muscle fascia. This distinction helps to explain why superficial veins can be treated by sclerotherapy without damage to the larger veins.
Veins contain one-way valves that push blood inward and upward toward the heart when they are functioning normally. The blood pressure in the superficial veins is usually low, but if it rises and remains at a higher level over a period of time, the valves in the veins begin to fail and the veins dilate, or expand. Veins that are not functioning properly are said to be "incompetent." As the veins expand, they become more noticeable because they lie closer to the surface of the skin, forming the typical patterns seen in spider veins.
Some people are at greater risk for developing spider veins. These risk factors include:
- Sex. Females in any age group are more likely than males to develop spider veins.
- Genetic factors. Some people have veins with abnormally weak walls or valves. They may develop spider veins even without a rise in blood pressure in the superficial veins.
- Pregnancy. A woman's total blood volume increases during pregnancy, which increases the blood pressure in the venous system. In addition, the hormonal changes of pregnancy cause the walls and valves in the veins to soften.
- Using birth control pills.
- Obesity. Excess body weight increases pressure on the veins.
- Occupational factors. People whose jobs require standing or sitting for long periods of time without the opportunity to walk or move around are more likely to develop spider veins than people whose jobs allow more movement.
- Trauma. Falls, deep bruises, cuts, or surgical incisions may lead to the formation of spider veins in or near the affected area.
As of 2003, there is no known method to prevent the formation of spider veins.
Sclerotherapy procedures
In typical outpatient sclerotherapy treatment, the patient changes into a pair of shorts at the doctor's office and lies on an examination table. After cleansing the skin surface with an antiseptic, the doctor injects a sclerosing agent into the veins. This agent is eliminated when the skin is stretched tightly over the area with the other hand. The doctor first injects the larger veins in each area of the leg, then the smaller ones. In most cases, one injection is needed for every inch of spider vein; a typical treatment session will require five to 40 separate injections. No anesthetic is needed for sclerotherapy, although the patient may feel a mild stinging or burning sensation at the injection site.
The liquid sclerosing agents that are used most often to treat spider veins are polidocanol (aethoxysklerol), sodium tetradecyl sulfate, and saline solution at 11.7% concentration. Some practitioners prefer to use saline because it does not cause allergic reactions. The usual practice is to use the lowest concentration of the chemical that is still effective in closing the veins.
A newer type of sclerosing agent is a foam instead of a liquid chemical that is injected into the veins. The foam has several advantages: It makes better contact with the wall of the vein than a liquid sclerosing agent; it allows the use of smaller amounts of chemical; and its movement in the vein can be monitored on an ultrasound screen. Sclerosing foam has been shown to have a high success rate with a lower cost, and causes fewer major complications.
After all the veins in a specific area of the leg have been injected, the doctor covers the area with a cotton ball or pad and compression tape. The patient may be asked to wait in the office for 20–30 minutes after the first treatment session to ensure that there is no hypersensitivity to the sclerosing chemicals. Most sclerotherapy treatment sessions are short, lasting from 15 to 45 minutes.
It is not unusual for patients to need a second treatment to completely eliminate the spider veins; however, it is necessary to wait four to six weeks between procedures.
Diagnosis/Preparation
Diagnosis
The most important aspect of diagnosis prior to undergoing sclerotherapy is distinguishing between telangiectasias and large varicose veins, and telangiectasias and spider nevi. Because sclerotherapy is intended to treat only small superficial veins, the doctor must confirm that the patient does not have a more serious venous disorder.
Spider nevi, which are also called "spider angiomas," are small, benign reddish lesions that consist of a central arteriole, which is a very small branch of an artery with smaller vessels radiating from it. Although the names are similar, spider nevi occur in the part of the circulatory system that carries blood (away) from the heart, whereas spider veins occur in the venous system that returns blood to the heart. To distinguish between the two, the doctor will press gently on the spot in the center of the network. A spider nevus will blanch, or lose its reddish color, when the central arteriole is compressed. When the doctor releases the pressure, the color will return. Spider veins are not affected by compression in this way. In addition, spider nevi occur most frequently in children and pregnant women, rather than in older adults. They are treated by laser therapy or electrodesiccation, rather than by sclerotherapy.
After taking the patient's medical history, the doctor examines the patient from the waist down, both to note the location of spider veins and to palpate (touch with gentle pressure) them for signs of other venous disorders. Ideally, the examiner will have a small raised platform for the patient to stand on during the examination. The doctor will ask the patient to turn slowly while standing, and will be looking for scars or other signs of trauma, bulges in the skin, areas of discolored skin, or other indications of chronic venous insufficiency. While palpating the legs, the doctor will note areas of unusual warmth or soreness, cysts, and edema (swelling of the soft tissues due to fluid retention). Next, the doctor will percuss certain parts of the legs where the larger veins lie closer to the surface. By gently tapping or thumping on the skin over these areas, the doctor can feel fluid waves in the veins and determine whether further testing for venous insufficiency is required. If the patient has problems related to large varicose veins, these must be treated before sclerotherapy can be performed to eliminate spider veins.
Some conditions and disorders are considered contraindications for sclerotherapy:
- Pregnancy and lactation. Pregnant women are advised to postpone sclerotherapy until at least three months after the baby is born, because some spider veins will fade by themselves after delivery. Nursing mothers should postpone sclerotherapy until the baby is weaned because it is not yet known whether the chemicals used in sclerotherapy may affect the mother's milk.
- Diabetes.
- A history of AIDS, hepatitis, syphilis, or other diseases that are carried in the blood.
- Heart conditions.
- High blood pressure, blood clotting disorders, and other disorders of the circulatory system.
Preparation
Patients are asked to discontinue aspirin or aspirin-related products for a week before sclerotherapy. Further, they are told not to apply any moisturizers, creams, tanning lotions, or sunblock to the legs on the day of the procedure. Patients should bring a pair of shorts to wear during the procedure, as well as compression stockings and a pair of slacks or a long skirt to cover the legs afterwards.
Most practitioners will take photographs of the patient's legs before sclerotherapy to evaluate the effectiveness of treatment. In addition, some insurance companies request pretreatment photographs for documentation purposes.
Aftercare
Aftercare following sclerotherapy includes wearing medical compression stockings that apply either 20–30 mmHg or 30–40 mmHg of pressure for at least seven to 10 days (preferably four to six weeks) after the procedure. Wearing compression stockings minimizes the risk of edema, discoloration, and pain. Fashion support stockings are a less acceptable alternative because they do not apply enough pressure to the legs.
The surgical tape and cotton balls used during the procedure should be left in place for 48 hours after the patient returns home.
Patients are encouraged to walk, ride a bicycle, or participate in other low-impact forms of exercise (examples: yoga and tai chi) to prevent the formation of blood clots in the deep veins of the legs. They should, however, avoid prolonged periods of standing or sitting, and such high-impact activities as jogging.
Risks
Cosmetically, the chief risk of sclerotherapy is that new spider veins may develop after the procedure. New spider veins are dilated blood vessels that can form when some of the venous blood forms new pathways back to the larger veins; they are not the original blood vessels that were sclerosed. Some patients may develop telangiectatic matting, which is a network of new spider veins that surface around the treated area. Telangiectatic matting usually clears up by itself within three to 12 months after sclerotherapy, but it can also be treated with further sclerosing injections.
Other risks of sclerotherapy include:
- Venous thrombosis. A potentially serious complication, thrombosis refers to the formation of blood clots in the veins.
- Severe inflammation.
- Pain after the procedure lasting several hours or days. This discomfort can be eased by wearing medical compression stockings and by walking briskly.
- Allergic reactions to the sclerosing solution or foam.
- Permanent scarring.
- Loss of feeling resulting from damage to the nerves in the treated area.
- Edema (swelling) of the foot or ankle. This problem is most likely to occur when the foot or ankle is treated for spider veins. The edema usually resolves within a few days or weeks.
- Brownish spots or discoloration in the skin around the treated area. These changes in skin color are caused by deposits of hemosiderin, which is a form of iron that is stored within tissue cells. The spots usually fade after several months.
- Ulceration of the skin. This complication may result from reactive spasms of the blood vessels, the use of overly strong sclerosing solutions, or poor technique in administering sclerotherapy. It can be treated by diluting the sclerosing chemical with normal saline solution.
- Hirsutism. Hirsutism is the abnormal growth of hair on the area treated by sclerotherapy. It usually develops several months after treatment and goes away on its own. It is also known as hypertrichosis.
Normal results
Normal results of sclerotherapy include improvement in the external appearance of the legs and relief of aching or cramping sensations associated with spider veins. It is common for complete elimination of spider veins to require three to four sclerotherapy treatments.
Morbidity and mortality rates
Mortality associated with sclerotherapy for spider veins is almost 0% when the procedure is performed by a competent doctor. The rates of other complications vary somewhat, but have been reported as falling within the following ranges:
- Hemosiderin discoloration: 10%–80% of patients, with fewer than 1% of cases lasting longer than a year.
- Telangiectatic matting: 5%–75% of patients.
- Deep venous thrombosis: Fewer than 1%.
- Mild aching or pain: 35%–55%.
- Skin ulceration: About 4%.
Alternatives
Conservative treatments
Patients who are experiencing some discomfort from spider veins may be helped by any or several of the following approaches:
- Exercise. Walking or other forms of exercise that activate the muscles in the lower legs can relieve aching and cramping because these muscles keep the blood moving through the leg veins. One exercise that is often recommended is repeated flexing of the ankle joint. By flexing the ankles five to 10 times every few minutes and walking around for one to two minutes every half hour throughout the day, the patient can prevent the venous congestion that results from sitting or standing in one position for hours at a time.
- Avoiding high-heeled shoes. Shoes with high heels do not allow the ankle to flex fully when the patient is walking. This limitation of the range of motion of the ankle joint makes it more difficult for the leg muscles to contract and force venous blood upwards toward the heart.
- Elevating the legs for 15–30 minutes once or twice a day. This change of position is frequently recommended for reducing edema of the feet and ankles.
- Wearing compression hosiery. Compression benefits the leg veins by reducing inflammation as well as improving venous outflow. Most manufacturers of medical compression stockings now offer some relatively sheer hosiery that is both attractive and that offers support.
- Medications. Drugs that have been used to treat the discomfort associated with spider veins include nonsteroidal anti-inflammatory drugs (NSAIDs) and preparations of vitamins C and E. One prescription medication that is sometimes given to treat circulatory problems in the legs and feet is pentoxifylline, which improves blood flow in the smaller capillaries. Pentoxifylline is sold under the brand name Trendar.
If appearance is the patient's primary concern, spider veins on the legs can often be covered with specially formulated cosmetics that come in a wide variety of skin tones. Some of these preparations are available in waterproof formulations for use during swimming and other athletic activities.
Electrodesiccation, laser therapy, and pulsed light therapy
Electrodesiccation is a treatment modality whereby the doctor seals off the small blood vessels that cause spider veins by passing a weak electric current through a fine needle to the walls of the veins. Electrodesiccation seems to be more effective in treating spider veins in the face than in treating those in the legs; it tends to leave pitted white scars when used to treat spider veins in the legs or feet.
Laser therapy, like electrodesiccation, works better in treating facial spider veins. The sharply focused beam of intense light emitted by the laser heats the blood vessel, causing the blood in it to coagulate and close the vein. Various lasers have been used to treat spider veins, including argon, KTP 532nm, and alexandrite lasers. The choice of light wavelength and pulse duration are based on the size of the vein to be treated. Argon lasers, however, have been found to increase the patient's risk of developing hemosiderin discoloration when used on the legs. The KTP 532nm laser gives better results in treating leg spider veins, but is still not as effective as sclerotherapy.
Intense pulsed light (IPL) systems differ from lasers because the light emitted is noncoherent and not monochromatic. The IPL systems enable doctors to use a wider range of light wavelengths and pulse frequencies when treating spider veins and such other skin problems, as pigmented birthmarks. This flexibility, however, requires considerable skill and experience on the part of the doctor to remove spider veins without damaging the surrounding skin.
Complementary and alternative (CAM) treatments
According to Dr. Kenneth Pelletier, the former director of the program in complementary and alternative treatments at Stanford University School of Medicine, California, horse chestnut extract is as safe and effective as compression stockings when used as a conservative treatment for spider veins. Horse chestnut ( Aesculus hippocastanum ) has been used in Europe for some years to treat circulatory problems in the legs; most recent research has been conducted in Great Britain and Germany. The usual dosage is 75 mg twice a day, at meals. The most common side effect of oral preparations of horse chestnut is occasional indigestion in some patients.
Resources
books
Pelletier, Kenneth R., M.D. The Best Alternative Medicine , Part II, "CAM Therapies for Specific Conditions: Varicose Veins." New York: Simon & Schuster, 2002.
"Varicose Veins." Section 16, Chapter 212 in The Merck Manual of Diagnosis and Therapy , edited by Mark H. Beers, M.D., and Robert Berkow, M.D. Whitehouse Station, NJ: Merck Research Laboratories, 1999.
periodicals
Brunnberg, S., S. Lorenz, M. Landthaler, and U. Hohenleutner. "Evaluation of the Long Pulsed High Fluence Alexandrite Laser Therapy of Leg Telangiectasia." Lasers in Surgery and Medicine 31 (2002): 359-362.
Crowe, Mark A., M.D. "Nevus Araneus (Spider Nevus)." eMedicine , April 12, 2002 [April 11, 2003]. http://www.emedicine.com/derm/topic293.htm .
Feied, Craig, M.D., Robert Weiss, M.D., and Robert B. Hashemiyoon, M.D. "Varicose Veins and Spider Veins." eMedicine , November 20, 2001 [April 10, 2003]. http://www.emedicine.com/derm/topic475.htm .
Frullini, A., and A. Cavezzi. "Sclerosing Foam in the Treatment of Varicose Veins and Telangiectases: History and Analysis of Safety and Complications." Dermatologic Surgery 28 (January 2002): 11-15.
Goldman, M. P. "Treatment of Varicose and Telangiectatic Leg Veins: Double-Blind Prospective Comparative Trial Between Aethoxyskerol and Sotradecol." Dermatologic Surgery 28 (January 2002): 52-55.
Kern, P. "Sclerotherapy of Varicose Leg Veins. Technique, Indications, and Complications." International Angiology 21 (June 2002): 40-45.
Loo, W. J., and S. W. Lanigan. "Recent Advances in Laser Therapy for the Treatment of Cutaneous Vascular Disorders." Lasers in Medical Science 17 (2002): 9-12.
MacKay, D. "Hemorrhoids and Varicose Veins: A Review of Treatment Options." Alternative Medicine Review 6 (April 2001): 126-140.
Pittler, M. H., and E. Ernst. "Horse-Chestnut Seed Extract for Chronic Venous Insufficiency. A Criteria-Based Systematic Review." Archives of Dermatology 134 (November 1998): 1356-1360.
Raulin, C., B. Greve, and H. Grema. "IPL Technology: A Review." Lasers in Surgery and Medicine 32 (2003): 78-87.
organizations
American Academy of Dermatology. 930 East Woodfield Rd., PO Box 4014, Schaumburg, IL 60168. (847) 330-0230. http://www.aad.org .
American Association for Vascular Surgery (AAVS). 900 Cummings Center, #221-U, Beverly, MA 01915. http://www.aavs.vascularweb.org .
American College of Phlebology. 100 Webster Street, Suite 101, Oakland, CA 94607-3724. (510) 834-6500. http://www.phlebology.org .
American Society of Plastic Surgeons (ASPS). 444 East Algonquin Road, Arlington Heights, IL 60005. (847) 228-9900. http://www.plasticsurgery.org .
Peripheral Vascular Surgery Society (PVSS). 824 Munras Avenue, Suite C, Monterey, CA 93940. (831) 373-0508. http://www.pvss.org .
other
American Society of Plastic Surgeons. Procedures: Sclerotherapy . [cited April 10, 2003]. http://www.plasticsurgery.org/public_education/procedures/Sclerotherapy.cfm .
Feied, Craig, M.D. Venous Anatomy and Physiology . [cited April 10, 2003] http://www.phlebology.org/syllabus1.htm .
Fronek, Helane S., M.D. Conservative Therapy for Venous Disease . [cited April 10, 2003] http://www.phlebology.org/syllabus4.htm .
Goldman, M. P., M.D. Complications of Sclerotherapy . [cited April 10, 2003] http://www.phlebology.org/syllabus9.htm .
Marley, Wayne, M.D. Physical Examination of the Phlebology Patient . [cited April 10, 2003] http://www.phlebology.org/syllabus2.htm .
Sadick, Neil S., M.D. Technique for Treating Telangiectasias and Reticular Veins. [cited April 10, 2003] http://www.phlebology.org/syllabus6.htm .
Weiss, Robert A., M.D., and Mitchel P. Goldman, M.D. Treatment of Leg Telangiectasias with Lasers and High-Intensity Pulsed Light . [cited April 10, 2003] http://www.phlebology.org/syllabus10.htm .
Rebecca Frey, Ph.D.
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Sclerotherapy is usually performed by general surgeons, dermatologists, or plastic surgeons, but it can also be done by family physicians or naturopaths who have been trained to do it. The American College of Phlebology holds workshops and intensive practical courses for interested practitioners. The ACP can be contacted for a list of members in each state.
Sclerotherapy is done as an outpatient procedure, most often in the doctor's office or in a plastic surgery clinic.
QUESTIONS TO ASK THE DOCTOR
- How likely am I to develop new spider veins in the treated areas?
- Do you use the newer sclerosing foams when you administer sclerotherapy?
- What technique(s) do you prefer to use for sclerotherapy and why?
it was the most painful thing I have ever experienced. I was literally lying there shaking and sweating. The pain from this procedure was unbearable and I almost stopped the session a few times. After the procedure I had severe pain in my right leg, and now its keeping me awake at night. I'm going to make an appointment to see someone, because it is becoming unbearable. I literally scream out at times..the pain can be so sharp. What a horrible experience!
Iam Ayman Abdelmofeed assistant lecturer of general surgery .
. Benha faculty of medicine –Cairo -Egypt
I have finished my master degree 2 years ago . I have got a scholarship
For doctoral degree in spider vien microsclerotherapy on the expenses
Of my university for any financial demands.
I need from you an acceptance to complete this research under your
supervision abroad and I need some papers on this subject .
Thanks
Ayman Abdelmofeed
I have had exactly the same experience as you. Had some spider veins treated some years ago without any problems. A month ago I went to a different doctor who first injected the "feeder veins" before treating the smaller spider veins (which seemed like a good idea to me then). The procedure itself was not that painful, but I got serious cramping and pain afterwards. I still have pain and cramping in my leg (4 weeks later) and wonder whether this will ever go away. To make things worse, the cosmetic results of the treatment were bad to. Many new spider veins have developed in my leg that weren't there before and my leg is swollen.
If you are still following this thread, Sherry, I would be interested to hear what you experiences in the meantime have been.
Good luck!
I went to a mediclinic and got penicillin and advil. It is not much better and the prescription is done today. I have trouble walking on it. Wonder if I should be worrying or not. The articles say one day recovery if that, well it is over a week. does anyone have any advice, because I would appreciate it. Oh and I do wear the stupid overpriced stockings.
my consultant said he had never heard of the problem before.
has anyone else had the same problem
I was curious to see if other doctors were doing the same thing.
I have had several treatments; sometimes seven or eight on one leg at a time. It has relieved the pain in my feet and legs.
I am so glad that my doctor suggested doing this.
I totally understand what you mean about doctors closing doors on you. I am also experiencing this now. To cut a long story short I am going through a similar thing, but not yet as severe as what you have experienced but is worsening by the day pain wise. I have been treated terribly by doctors, but a highly regarded specialist has admitted negligence has occurred and is willing to back me. I did write you a very lenghty message but lost the whole lot. If you read this I can tell you in detail the channels i went through to get answers. This happened the other day and i'm hoping justice will prevail now and I can now get proper treatment.
Fiona
Laura in CA