Pyloroplasty
Definition
Pyloroplasty is a surgical procedure in which the pylorus valve at the lower portion of the stomach is cut and resutured, relaxing and widening its muscular opening (pyloric sphincter) into the duodenum (first part of the small intestine). Pyloroplasty is a treatment for patients at high risk for gastric or peptic ulcer disease (PUD).
Purpose
Pyloroplasty surgery enlarges the opening through which stomach contents are emptied into the intestine, allowing the stomach to empty more quickly. A pyloroplasty is performed to treat the complications of PUD or when medical treatment has not been able to control PUD in high-risk patients.
Demographics
Nearly four million people in the United States have PUD; about five adults in 100,000 will develop an ulcer. About 1.7% of children being treated in general pediatric practices are diagnosed with PUD. The presence of ulcer-causing Helicobacter pylori bacteria occurs in 10% of the population in industrialized countries and is believed to cause 80–90% of primary ulcers. In the United States, H. pylori infection occurs more frequently in black and Hispanic populations than in white. The frequency of secondary ulcers (caused by other existing conditions) is not known as it depends on the frequency of other illnesses, chronic diseases, and drug use. Primary and secondary PUD can occur in patients of all ages. Primary PUD is rare in children under age 10, increasing during adolescence. Secondary PUD is more prevalent in children under age six.
Description
Peptic ulcer disease develops when there is an imbalance between normal conditions that protect the lining (mucosa) of the stomach and the intestines and conditions that disrupt normal functioning of the lining. Protective factors include the water-soluble mucosal gel layer, the production of bicarbonate in the lining to balance acidity, the regulation of gastric acid (stomach acid) secretion, and blood flow in the lining. The aggressive factors that work against this protective gastric-wall system are excessive acid production, H. pylori bacterial infection, and a reduced blood flow (ischemia) in the mucosal lining. These aggressive factors can cause inflammation and ulcer development. A peptic ulcer is a type of sore or hole (perforation) that forms on the lining of the stomach (gastric ulcer) or intestine (duodenal ulcer), when the lining has been eaten away by stomach acid and digestive juices. Peptic ulcers can be primary, caused by H. pylori infection, or secondary, caused by excess acid production, stress, use of medications, and other underlying
Other factors that contribute to mucosal inflammation and ulceration include:
- alcohol and caffeine use
- non-steroidal anti-inflammatory drugs (NSAIDs)
- aspirin
- cigarette smoking
- exposure to certain irritating chemicals
- emotional disturbances and prolonged stress
- traumatic injuries and burns
- respiratory failure
- blood poisoning
- critical illnesses that create imbalances in body chemistry
Symptoms of gastric or peptic ulcer include burning pain, nausea, vomiting, loss of appetite, bloating, burping, and losing weight.
When PUD is diagnosed or high risk established, medical treatment will begin to treat H. pylori infection if present and to restore balanced conditions in the mucosal lining. Any underlying condition may be treated simultaneously, including respiratory disorders, fluid imbalance, or stomach and digestive disorders. Medications may be prescribed to help correct gastric disturbances and control gastric acid secretion. Certain drugs that are prescribed for other conditions, especially NSAIDs, may be discontinued if they are known to cause inflammation. Adult patients may be advised to discontinue alcohol and caffeine use and to stop smoking.
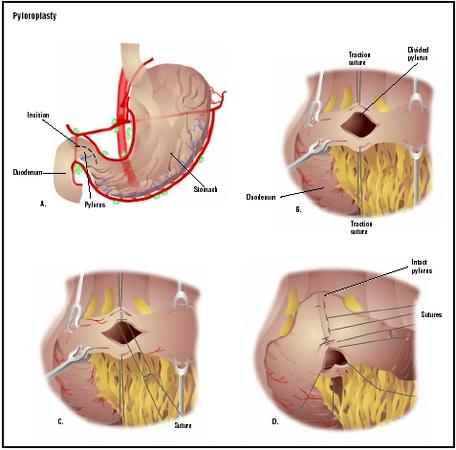
When medical treatment alone is not able to improve the conditions that cause PUD, a pyloroplasty procedure may be recommended, particularly for patients with stress ulcers, perforation of the mucosal wall, and gastric outlet obstruction. The surgery involves cutting the pylorus lengthwise and resuturing it at a right angle across the cut to relax the muscle and create a larger opening from the stomach into the intestine. The enlarged opening allows the stomach to empty more quickly. A pyloroplasty is sometimes done in conjunction with a vagotomy procedure in which the vagus nerves that stimulate stomach acid production and gastric motility (movement) are cut. This may delay gastric emptying and pyloroplasty will help correct that effect.
Diagnosis
Diagnosis begins with an accurate history of prior illnesses and existing medical conditions as well as a family history of ulcers or other gastrointestinal (stomach and intestines) disorders. A complete history and comprehensive diagnostic testing may include:
- location, frequency, duration, and severity of pain
- vomiting and description of gastric material
- bowel habits and description of stool
- all medications, including over-the-counter products
- appetite, typical diet, and weight changes
- family and social stressors
- alcohol consumption and smoking habits
- heart rate, pulse, and blood pressure
- chest examination and x ray, if necessary
- palpation (touch) of the abdomen
- rectal examination and stool testing
- pelvic examination in sexually active females
- examination of testicles and inguinal (groin) area in males
- testing for the presence of Helicobacter pylori
- complete blood count and blood chemistry profile
- urinalysis
- imaging studies of gastrointestinal system (x ray, other types of scans)
- biopsy of stomach lining using a tube-like telescopic instrument (endoscope)
Preparation
Before surgery, standard preoperative blood and urine tests will be performed and various x rays may be ordered. The patient will not be permitted to eat or drink anything after midnight the night before the procedure. When the patient is admitted to the hospital, cleansing enemas may be ordered to empty the intestine. If nausea or vomiting are present, a suction tube may be used to empty the stomach.
Aftercare
The patient will spend several hours in a recovery area after surgery where blood pressure, pulse, respiration, and temperature will be monitored. The patient's breathing may be shallower than normal because of the effect of anesthesia and the patient's reluctance to breathe deeply and experience pain at the site of the surgical incision. The patient will be shown how to support the site while breathing deeply or coughing, and will be given pain medication as needed. Fluid intake and output will be measured. The operative site will be observed for any sign of redness, swelling, or wound drainage. Intravenous fluids are usually given for 24–48 hours until the patient is gradually permitted to eat a special light diet and as bowel activity resumes. About eight hours after surgery, the patient may be allowed to walk a little, increasing movement gradually over the next few days. The average hospital stay, dependent upon the patient's overall recovery status and any underlying conditions, ranges from six to eight days.
Risks
Potential complications of this abdominal surgery include excessive bleeding, surgical wound infection, incisional hernia, recurrence of gastric ulcer, chronic diarrhea, and malnutrition. After the surgery, the surgeon should be informed of an increase in pain, and of any swelling, redness, drainage, or bleeding in the surgical area. The development of headache, muscle aches, dizziness, fever, abdominal pain or swelling, constipation, nausea or vomiting, rectal bleeding, or black stools should also be reported.
Normal results
Complete healing is expected without complications. Recovery and a return to normal activities should take from four to six weeks.
Morbidity and mortality rates
Successful treatment of Helicobacter pylori has improved morbidity and mortality rates, and the prognosis for PUD, with proper treatment and avoidance of causative factors, is excellent. Pyloroplasty is rarely performed in primary ulcer disease. Morbidity and mortality are higher in patients with secondary ulcers because of underlying illness that complicates both PUD and surgical treatment.
Resources
books
Monahan, Frances. Medical-Surgical Nursing. Philadelphia: W. B. Saunders Co., 1998.
organizations
American Gastroenterological Association. 7910 Woodmont Ave., Seventh Floor, Bethesda, MD 20814. (301) 654-2055. http://www.gastro.org .
National Institute of Diabetes and Digestive and Kidney Disorders. 31 Center Drive, Bethesda, MD 20892. (301) 496-7422. http://www.niddk.nih.gov .
other
"Peptic Ulcer Surgery." Mayo Clinic Online. March 5, 1998. http://www.mayohealth.org .
"Peptic Ulcer Disease." Inteli Health. Harvard Medical School and Aetna Consumer Health Information. March 6, 2001. http://www.intelihealth.com .
Kathleen D. Wright, RN L. Lee Culvert
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
A pyloroplasty surgery is performed by a general surgeon in a hospital or medical center operating room .
QUESTIONS TO ASK THE DOCTOR
- How will this surgery be performed?
- What is your experience with this procedure? How often do you perform this procedure?
- Why must I have the surgery?
- What are my options if I opt not have the surgery?
- How can I expect to feel after surgery?
- What are the risks involved in having this surgery?
- How quickly will I recover? When can I return to school or work?
- What are my chances of getting this condition again?
- What can I do to avoid getting this condition again?
My question is: My wife has had radiation and chemo treatments for Adult Wilms Tumor in 2000 and 2001. She had the Lt kidney removed, a G.B. Removed, and a Lt Hemicolectomy. Since then a gradual shift of the stomach has taken place. She now gets periodic episodes of a Sm. Bowel obstruction. Each episode is closer together, lasts longer, and she is less able to tol. solid foods. We have been through the mill of tests, exams, CT scans, MRI's, Consults etc etc.. We need some answeres as to whether this proceedure (pyloroplasty will help to straighten out a shifted stomach, which in turn cincks the pyloric valve, and the sm. intestine.
Plrease refer me to the EXPERTS on this tough and difficult issue for my wife and I.
Thank You,
Bill Westphal RN Surg. Dept. whwesty@hotmail.com
is recovery time lengthy and if i already have malabsorption issues should i go through with this
I would appreciate any information.
Thank you
I am 40 years old. I have been suffering stomack irritation last 20years back. Doctor has given lot of medicine but now I am taking Rebeparazole, esomeparazole etc but I can't control irritaion by the medicine. Now, i am decide to do highly selective vagotomy. Would you Please advise advantage and disadvantage. I am really puzzle. Thanks, Monir
I am suffering gastratis last twenty years. doctor has given lot of medecine to reduce the acid secretion but now medecine is not and can't control my burning in stomach. I am only 40 years old and now I am taking Lansoperazole-30mg three time and with sucralfate and domperidon. but the result is zero. i have done endoscopy four time but did not find out any ulceration in my stomach. So What i should do??? some time I think to do highly selective vegatomy. Would please advice me how control my irritation. I am very very worried because I have sdmall two sons. i can't work properly. I am waiting for your good advise sir.
I recommend looking at your life, taking care of eating right, read and study because surgery is only a band aid you have to give your body a chance to function and even heal itself. I am very sorry I had this surgery and wish I had changed my life and taken the stress away instead. Every individuals problems are different- but it is meant to have the enzymes in the stomach and those are non existant after a few years with the surgery. I found I was starving to death. Enzymes have helped me with the pain and discomfort lately.
Thank you