Ileoanal anastomosis
Definition
Ileoanal anastomosis is a surgical procedure in which the large intestine is bypassed and the lower portion of the small intestine is directly attached to the anal canal. It is also called an ileal pouch-anal anastomosis.
Purpose
An ileoanal anastomosis is an invasive procedure performed in patients who have not responded to more conservative treatments. The small intestine is composed of three major sections: the duodenum, which is the upper portion into which the stomach empties; the jejunum, which is the middle portion; and the ileum. The ileum is the last portion of the small intestine and empties into the large intestine. The large intestine is composed of the colon, where stool is formed, and the rectum, which empties to the outside of the body through the anal canal.
Surgical removal of the bowel is usually a procedure of last resort for a patient who has not responded to less invasive medical therapies. For example, many patients with ulcerative colitis, an inflammatory condition of the colon and rectum, can be treated by medications or dietary changes that control the symptoms of the disease. For patients who fail to respond to these approaches, however, the creation of an ileoanal anastomosis removes most or all of the diseased tissue. Certain types of colon cancer and a condition called familial adenomatous polyposis, or FAP, in which the inner lining of the colon becomes covered with abnormal growths, may also be treated with ileoanal anastomosis.
Demographics
Most patients—more than 85%—who undergo an ileoanal anastomosis are being treated for ulcerative colitis; familial adenomatous polyposis is the next most common condition requiring the surgery. The average age of patients at surgery is 35 years, and the majority of patients are male.
Description
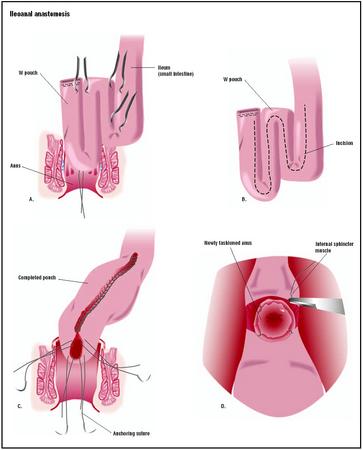
A surgical anastomosis is the connection of two cut or separate tubular structures to make a continuous channel. To perform an ileoanal anastomosis, the surgeon detaches the ileum from the colon and the anal canal from the rectum. He or she then creates a pouch-like structure from ileal tissue to act as a rectum and connects it directly to the anal canal. This procedure offers distinct advantages over a conventional ileostomy , a procedure in which the ileum is connected to the abdominal wall. A conventional ileostomy leaves the patient incontinent (i.e., unable to control the emptying of waste from the body) and unable to have normal bowel movements. Instead, the patient's waste is excreted through an opening in the abdominal wall into a bag. An ileoanal anastomosis, however, removes the diseased large intestine while allowing the patient to pass stool normally without the need of a permanent ileostomy.
An ileoanal anastomosis is usually completed in two separate surgeries. During the first operation, the surgeon makes a vertical incision through the patient's abdominal wall and removes the colon. This procedure is called a colectomy. The inner lining of the rectum is also removed in a procedure called a mucosal proctectomy. The muscles of the rectum and anus are left in place so that the patient will not be incontinent. Next, the surgeon makes a pouch by stapling sections of the small intestine together with surgical staples. The pouch may be J-, W-, or S-shaped, and acts as reservoir for waste (as the rectum does) to decrease the frequency of the patient's bowel movements. Once the pouch is constructed, it is connected to the anal canal to form the anastomosis. To allow the anastomosis time to heal before stool begins to pass through, the surgeon creates a temporary "loop" ileostomy. The surgeon then makes a small incision through the abdominal wall and brings a loop of the small intestine through the incision and sutures it to the skin. Waste then exits the body through this opening, which is called a stoma, and collects in a bag attached to the outside of the abdomen. In an emergency situation, the surgeon may perform the colectomy and ileostomy during one operation, and create the ileal pouch during another.
In the second operation, the surgeon closes the ileostomy, thus restoring the patient's ability to defecate in the normal manner. This second procedure generally takes place two to three months after the original surgery. The surgeon detaches the ileum from the stoma and attaches it to the newly created pouch. A continuous channel then
Diagnosis/Preparation
Because an ileoanal anastomosis is a procedure that is done after a patient has failed to respond to other therapies, the patient's condition has been diagnosed by the time the doctor suggests this surgery.
The patient meets with the operating physician prior to surgery to discuss the details of the surgery and receive instructions on pre- and post-operative care. Immediately before the operation, an intravenous (IV) line is placed in the patient's arm to administer fluid and medications, and the patient is given a bowel preparation to cleanse the bowel for surgery. The location of the stoma is marked on the skin so that it is placed away from bones, abdominal folds, and scars.
Aftercare
Following surgery, the staff will instruct the patient in the care of the stoma, placement of the ileostomy bag, and necessary changes regarding diet and lifestyle. Visits with an enterostomal therapist (ET) or a support group for individuals with ostomies may be recommended to help the patient adjust to living with a stoma. After the anastomosis has healed, which usually takes about two to three months, the ileostomy can then be closed. A dietician may suggest permanent changes in the patient's diet to minimize gas and diarrhea.
Risks
Risks associated with any surgery that involves opening the abdomen include excessive bleeding, infection, and complications due to general anesthesia. Specific complications following an ileoanal anastomosis include leakage of stool, anal stenosis (narrowing of the anus), pouchitis (inflammation of the ileal pouch), and pouch failure. Patients who have received a temporary ileostomy may experience obstruction (blockage) of the stoma, stomal prolapse (protrusion of the ileum through the stoma), or a rash or skin irritation around the stoma.
Normal results
After ileoanal anastomosis, patients will usually experience between four and nine bowel movements during the day and one at night; this frequency generally decreases over time. Because of the nature of the surgery, persons with an ileoanal anastomosis retain the ability to control their bowel movements. They can refrain from defecating for extended periods of time, an advantage not afforded by a conventional ileostomy. One study found that 97% of patients were satisfied with the results of the surgery and would recommend it to others with similar disorders.
Morbidity and mortality rates
The overall rate of complications associated with ileoanal anastomosis is approximately 10%. Between 10% and 15% of patients will experience at least one episode of pouchitis, and 10–20% will develop postsurgical pelvic or wound infections. The rate of anastomosis failure requiring the creation of a permanent ileostomy is approximately 5–10%.
Alternatives
An ileostomy is a surgical alternative for patients who are not good candidates for an ileoanal anastomosis. If the patient wishes to retain continence, the surgeon may perform a continent ileostomy. Portions of the small intestine are used to form a pouch and valve; these are then directly attached to the abdominal wall skin to form a stoma. Waste collects inside the internal pouch and is expelled by insertion of a soft, flexible tube through the stoma several times a day.
Resources
books
Pemberton, John H., and Sidney F. Phillips. "Ileostomy and Its Alternatives." In Sleisenger and Fordtran's Gastrointestinal and Liver Disease , 7th ed. Philadelphia: Elsevier Science, 2002.
periodicals
Becker, James M. "Surgical Therapy for Ulcerative Colitis and Crohn's Disease." Gastroenterology Clinics of North America 28 (June 1, 1999): 371-90.
organizations
Crohn's and Colitis Foundation of America. 386 Park Ave. S., 17th Floor, New York, NY 10016. (800) 932-2423. http://www.ccfa.org .
United Ostomy Association, Inc. 19772 MacArthur Blvd., Suite 200, Irvine, CA 92612-2405. (800) 826-0826. http://www.uoa.org .
other
Hurst, Roger D. "Surgical Treatment of Ulcerative Colitis." Crohn's and Colitis Foundation of America. [cited May 1, 2003]. http://www.ccfa.org/medcentral/library/surgery/ucsurg.htm .
Stephanie Dionne Sherk
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Ileoanal anastomoses are usually performed in hospital operating rooms. They may be performed by a general surgeon, a colorectal surgeon (a medical doctor who focuses on diseases of the colon, rectum, and anus), or a gastrointestinal surgeon (a medical doctor who focuses on diseases of the gastrointestinal system).
QUESTIONS TO ASK THE DOCTOR
- Why are you recommending an ileoanal anastomosis?
- What type of pouch will be created?
- Will an ileostomy be created? When will it be reversed?
- Are there any nonsurgical alternatives to this procedure?
- When will I be able to resume my normal diet and activities?
I am very healthy.I take no supplements or vitamins.
I had UC for 13 years and took prednisone. No problems at all.
I try to help others get their quality of life back and I am an advocate for my son who had a failed j pouch and now has a continent ostomy.jpouch.org has great information to help.
He has confided in me that he has sperm stored.
What I wanted to ask is why he would have sperm stored? Is this related to the diabetes or the ulcerative colitis? Did anyone else have this offered or suggested to them prior to surgery?
Any advice would be awesome. melk@alpenglow.com.au
Good luck
Angie
Please email or contact me if you don't mind. I also welcome others' instructions about how to contact George. Thanks!
If you would like any more info feel free to email joconloz@hotmail.com
We have only been Married now for about 5 years and when I talk about his eating habits he tells me he needs to stay away from raw vegatables and fruit, and seeds. What I wnat to know is what other foods we need to avoid. Are there spices that I shouldn't use. How should I cook our food, and any other information that could be of use.
I am looking for some answers. I had rectal cancer. I had surgery to remove my rectom and reconstruct my colon. I got an infection after surgery which formed pouch full of fluid that needed to be drained. In Nov it will be 2 years. I have pain in my lower back, both sides of my butt, hips,and down the sides of my upper legs. Dr's tried to blame Chemo and radiation for this pain. I believe it is inflamation and or nerve damage. I take a nerve pain killer and lots and lots of ibprophen a few times a day. Now this wierd pouch is still not healed up, is inflammed and red. Could this be the cause of my pain?? How do I fix this problem? Both side of my pain areas are affected at the same time..chronic, constant aching/pain. I am cancer free now, but this pain is a constant reminder of my horrible fight with cancer.. Help.. any ideas?
I had the same problem after my surgery with my pouch filling with fluid, I was taken back to theatre 10 days post op, they drained 2 pints out in theatre and placed a drain inside me to drain the rest away. They sent some of the fluid away for testing and it came back that I had an infection called "esbl" in my pouch which I believe is a form of e-coli. I am pre takedown and am now suffering from pouchitis, again they have taken a sample and sent it away for testing. I only found this out yesterday after having an examination under anaesthetic due to suspected recto vaginal fistula (good news they didnt find one!). Has anyone had pouchitis pre takedown? Some sites say you cannot get it, if so what else could it be? My surgeries where for UC, although originally diagnosed with crohns, post colon removal testing came back UC.
Any advice etc, would be great.
Thanks
Michelle
Please e.mail if you can. Thanks Viv.
From the day I had my J-pouch I went to the loo 15-20 times a day. I took codeine phosphate, antibiotics etc. The codeine helped a little but seemed to give me stomach ache. In 2005 I started to get slow output but still frequency when the pouch would only empty a very small amount at a time. This made me very sore and I developed fissures. Then within one week the pouch suddenly stopped the output and I was in terrible pain. I was rushed to hospital, x-rayed, given a barium enema and sent home. This happened again 10 days later and again on three other occasions. Since that time in 2005 I have had to use a tube and irrigate at least twice a day, sometimes three. My surgeon says he cannot do anything about it. I could have an ileostomy but my skin becomes very sore and the loop will not stay one. I have also starting suffering with pain in the lower back, buttocks and down the side of both my legs. I cannot sit on a hard surface because the top of my legs and buttocks become painful. My doctor says I have some nerve damage.
It took me 6 months to care for myself alone and a year to get back to dancing. I never went back to College. I’d begun teaching (Stage Mothers!) when I received a special invite from Disney for the next season. I decided to go and out of a 3 month 3 show season. I danced 1 month, was hospitalized 2 weeks, off 2 more weeks, danced last month. I've never dance professionally again.
I’ve dealt with small bowel obstructions every 6 months or so, a 5-7 days 2in the hospital each episode. I’ve had 3 “ full openâ€adhesiolysis surgeries 11-14days in hospital each time, 2 “full open†small bowel resection surgeries,5 &7 resections respectively 17-23 days in hospital each episode.
No. I cannot eat anything I want. I eat plain yogurt, baby food, vanilla ice cream, white toast w butter, poached eggs , & mashed potatoes. That’s It! Anything else causes obstructions and or intolerable pain.
I have 11-12 toilette visits per day and 2-4 at night.
I cannot have children because of all the scar tissue. This is very common with this surgery.
Now 30+ years later I have intense pain from the scar tissue and nerve damage that I can’t work. I can paint for short periods. I put on my favorite music and let my paintbrush dance the canvas for my body that can’t dance the stage.
My best advice is be informed and objective in making your decision. Best Wishes Cris - Luv Jil
Karen
Because I'm now in my 30s I think about having kids. I will admit that I'm not dying to have children but I want to know if it's a good option for me. I will also admit that I'm worried about being pregnant and being in the care of a doctor that may want to cut me open (something I've become fearful of). In my investigation to figuring out my body (I'm an anatomy geek and believer in therapy outside of surgery and meds), I am trying to find out what is causing my menstrual cycle to last so long. I recently saw a craniosacral therapist whom I think is very good. She gently felt my belly and sensed that the scar tissue from the surgery is pulling my uterus away from center, where it should live. It's in a state of spasm and not functioning as it should, according to her. She also felt that overall my organs were adhered to one another, due to the scar tissue. She did some very gentle, subtle myofascial release (to loosen up the connective tissue). It didn't feel like she did much, although my belly did feel released/less tense. The next day, I had a rehearsal and I did some intense partnering work, where there was some pressure on my belly - but that's not out of the ordinary for me. But I realize now that's something I shouldn't have done. Something moved out of place, close to the surface, near my scar/belly button. It's been a month now and it still occasionally bothers me and causes some pain. Western doctors aren't worried about it and say it could be one of many things (scar tissue, residual staple, etc). They don't seem to think it's a hernia. Only an MRI could tell them for sure (and that's too $$ - I'm a modern dancer, we don't have proper healthcare benefits). In any case, whatever it is, it's inhibiting my dancing and I'm discouraged about it. I'm hoping the cransiosacral therapist can help me drop it back into place. But I have this feeling that I will have to figure out how to heal it on my own. If anyone has thoughts, please feel free to share.
Wishing good health to everyone!!
I am not that sure, but i think the surgery just alleviate the symtomps but the UC is still on your body. Because is auotimmune. I have no the Jpouch yet, because the doctors think that i have the Chron's disease. What i' going to do is keep the rectum with the hope that some day there is a cure. You should think twice if you want to remove everything, because, if you do, you won't have any hopes, even if a cure becomes.Wishing you the best! Cris
I have had pelvic floor disfunction for close to 8 years now, with it getting increasingly worse. I am been to numerous drs. and also to the mayo clinic for pelvic floor retraining. I have had a enterocele repair and rectoplexy done. I am still struggling daily to go to the bathroom but none of the muscles cooperate in my rectum, they tighten instead of opening. I am scheduled in a week to meet w/a surgeon to discuss Ileoanal surgery. If he doesn't think that will work I will have an illeostomy. My concern is that it won't work due to the fact that my pelvic floor and rectum do not work properly. Can anyone give advice on weather this won't be an issue or not. After suffering for so long I want to make the right decision with surgery, since last one gave me nerve damage which is just complicating things worse. Thank you for any advice given.
Also, i have the UC active on my rectum. The difference is that i dont have the J-pouch because of it. I am being treated with supoositories and I feel much better. The choice is only yours, but, I insist you should try everything you can to not remove the rectum. That's what i'm doing, beacuse, I want a life without the illeostomy. I hope you feel better, Cris.
Thanks, Susie
Well I have for two weeks now hou long is this going to last.
My stomach is so sore I'm so week and tired. Any answers out there please.
Did you guys get rectal leakage after the tubes were removed etc? How long did it go on for & is it supposed to hurt so much??
Im struggling with major nausea not even clopomin is helping anymore and its wrecking havoc on my weight. When i eat, a few bites feels like a full meal, when i swallow pills they gag up & i have to force them down with more water . Guys any tips & tricks on how to feel normal again during the first few weeks would be lifechanging really guys.