Ileal conduit surgery
Definition
There are many surgical techniques for urinary diversion surgery. They fall into two categories: continent diversion and conduit diversion. In continent diversion, also known as continent catheterizable stomal reservoir, a separate rectal reservoir for urine is created, which allows evacuation from the body. In conduit diversion, or orthotopic urethral anastomotic procedure, an intestinal stoma or conduit for release of urine is created in the abdominal wall so that a catheter or ostomy can be attached for the release of urine. An ileal conduit is a small urine reservoir that is surgically created from a small segment of bowel. Both techniques are forms of reconstructive surgery to replace the bladder or bypass obstructions or disease in the bladder so that urine can pass out of the body. Both procedures have been used for years and should be considered for all appropriate patients. Ileal conduit surgery, the easiest of the reconstructive surgeries, is the gold standard by which other surgical techniques, both continent and conduit, have been compared as the techniques have advanced over the decades.
Purpose
The bladder creates a reservoir for the liquid wastes created by the kidneys as a result of the ability of these organs to filter and retain glucose, salts, and minerals that the body needs. When the bladder must be removed; or becomes diseased, injured, obstructed, or develops leak points; the release of urinary wastes from the kidneys becomes impaired, endangering the kidneys with an overburden of poisons. Reasons for disabling the urinary bladder are: cancer of the bladder; neurogenic sources of bladder dysfunction; bladder sphincter detrusor overactivity that causes continual urge incontinence; chronic inflammatory diseases of the bladder; tuberculosis; and schistosomiasis, which is an infestation of the bladder by parasites, mostly occurring Africa and Asia. Radical cystectomy , removal of the bladder, is the predominant treatment for cancer of the bladder, with radiation and chemotherapy as other alternatives. In both cases, urinary diversion is often necessitated, either due to the whole or partial removal of the bladder or to damage done by radiation to the bladder.
Demographics
Urinary diversion has a long history and, over the last two decades, has developed new techniques for urinary tract reconstruction to preserve renal function and to increase the quality of life. A number of difficulties had to be solved for such progress to take place. Clean intermittent catherization by the patient became possible in the 1980s, and many patients with loss of bladder function were able to continue to have urine release through the use of catheters. However, it soon became clear that catherization left a residue that cumulatively, and over time, increased the risk of infection, which subsequently decreased kidney function through reflux, or backup, of urine into the kidneys. A new way had to be found. With the advent of surgical anatomosis (the grafting of vascularizing tissue for the repair and expansion of organ function) as well as with the ability to include a flap-type of valve to prevent backup, bladder reconstructive surgery that allowed for protection of the kidneys became possible.
Description
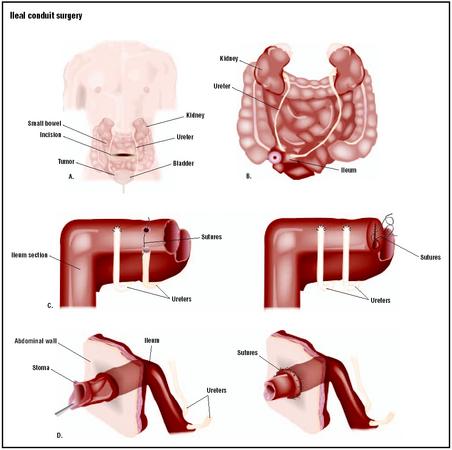
Ileal conduit surgery consists of open abdominal surgery that proceeds in the following three stages:
- Isolating the ileum, which is the last section of small bowel. The segment used is about 5.9–7.8 in (15–20 cm) in length.
- The segment is then anastomosized, or grafted, to the ureters with absorbable sutures.
- A stoma, or opening in skin, is created on the right side of the abdomen.
- The other end of the bowel segment is attached to the stoma, which drains into a ostomy bag.
Stents are used to bypass the surgical site and divert urine externally, ensuring that the anastomotic site has adequate healing time. Continent surgeries are more extensive than the ileal conduit surgery and are not described here. Both types of surgery require an extensive hospitalization with careful monitoring of the patient for infections, removal of stents placed in the bowel during surgery, and removal of catheters.
Diagnosis/Preparation
Ileal conduit surgery is recommended depending on what conditions are being treated; whether the urinary diversion is immediately necessary; for the relief of pain or discomfort; or for relatively healthy individuals or individuals with terminal illness. Three major decisions that must be made by the physician and patient include:
- The type of surgery to restore bladder function: either by sending urine through the ureters to a new repository fashioned in the rectum, or by creating a conduit for the removal of the urine out through the stomach wall and into a permanent storage pouch, or ostomy outside the body.
- The type of material out of which to fashion the reservoir or conduit.
- Where to place the stoma outlet for patient use.
Recent research has shown there is little difference in infection rates or in renal deterioration between the conduit surgical techniques and the continent techniques. The patient's preference becomes important as to which type of surgery and resulting procedures for urination they want. Of course, some patients, unable to conduct catheterization due to debilitating diseases like multiple sclerosis or neurological injuries, should be encouraged to have the reservoir or continent procedures.
Materials for fashioning continent channels have included sections of the appendix, stomach, ileum and cecum of the intestines, and for the reservoir, sigmoid and ureter tissues, usually with an anti-refluxing mechanism to maximize continence. A segment of the ileum is often preferred, unless the tissue has received radiation. In this case, other tissue must be used. Ileum is preferred because the ileal tissue of the intestines accommodates larger urine volume at lower pressure.
Many urinary diversion procedures are performed in conjunction with surgery for recurrent cancer or complications of pelvic radiation. Fistula development and repeated repair as well as ureteral obstruction also are reasons to have the surgery. If the surgery is considered because of cancer, the physician and the patient need to discuss how appropriate the surgery is for cure or for relieving pain. Highly relevant are the patient's age, medical condition, and ability to comprehend both the procedure and the patient's role in the changed state that will result with the surgery. In general, ileal conduit surgery is easier, faster, and has fewer complications than continent reservoir surgery.
In addition to these considerations, great emphasis must be put on preparing the patient psychologically, and physicians must make themselves available for counseling and questions before proceeding with patient evaluation for the procedures. The renal system must be assessed using pylography, which is the visualization of the renal pelvis of the kidneys to determine the health of each renal system. Patients with renal disease or abnormalities are not good candidates for urinary diversion. Bowel preparation and prophylactic antibiotics are necessary to avoid infection with the surgery. Bowel preparation includes injecting a clear-liquid diet preoperatively for two days, followed by using a cleansing enema or enemas until the bowel runs clear. The importance of these preparations must be explained to the patient: leaking from the bowel during surgery can be life threatening. For ileal conduits, the placement of the stoma must be decided. This is accomplished after the physician evaluates the patient's abdomen in both a sitting and standing position, to avoid placing the stoma in a fatty fold of the abdomen. The input from a stomal therapist is important for this preparation with the patient.
Aftercare
Ureteral stents are generally removed one week after surgery. A urine culture is taken from each stent.
Patients are taught how to care for the ostomy, and family members are educated as well. Appropriate supplies and a schedule of how to change the pouch are discussed, along with skin care techniques for the area surrounding the stoma. Often, a stomal therapist will make a home visit after discharge to help the patient return to normal daily activities.
Risks
This surgery includes the major risks of thrombosis and heart difficulties that can result from abdominal surgery. Many difficulties can occur after urinary diversion surgery, including urinary leakage, problems with a stoma, changes in fluid balance, and infections over time. However, urinary diversion is usually tolerated well by most patients, and reports indicate that patient satisfaction is very high. Common complications are stricture caused by inflammation or scar tissue from surgery, disease, or injury. The incidence of urine leakage for all types of ureterointestinal anastomoses is 3–5% and occurs within the first 10 days after surgery. According to some researchers, this incidence of leakage can be reduced to near zero if stents are used during surgery.
Normal results
Complete healing is expected without complications, with the patient returning to normal activities once they have recovered from surgery.
Morbidity and mortality rates
Possible complications associated with ileal conduit surgery include bowel obstruction, blood clots, urinary tract infection, pneumonia, skin breakdown around the stoma, stenosis of the stoma, and damage to the upper urinary tract by reflux. Pyelonephritis, or bacterial infection of a kidney, occurs both in the early postoperative period and over the long term. Approximately 12% of patients diverted with ileal conduits and 13% in those diverted with anti-refluxing colon conduits have this complication. Pyelonephritis is associated with significant mortality.
Alternatives
An alternative to ileal conduit surgery is continent surgery in which a neo-bladder is fashioned from bowel segments, allowing the patient to evacuate the urine and avoid having an external appliance. The procedures of continent diversion are more complicated, require more hospitalization, and have higher complication rates than conduit surgery. Many patients, unable to manage a stoma, are good candidates for continent diversion.
Resources
books
Walsh, P., et al. Campbell's Urology, 8th Edition. St. Louis: Elsevier, 2000.
periodicals
Estape, R., L. E. Mendez, R. Angioli, and M. Penalver. "Gynecologic Oncology: Urinary Diversion in Gynecological Oncology." Surgical Clinics of North America 81, no. 4 (August 2002).
organizations
National Digestive Diseases Information Clearinghouse. 2 Information Way, Bethesda, MD 20892-3570. http://www.niddk.nih.gov .
United Ostomy Association, Inc. (UOA). 19772 MacArthur Blvd., Suite 200, Irvine, CA 92612-2405. (800) 826-0826. http://www.uoa.org. .
Nancy McKenzie, PhD
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Surgery is performed by a urological surgeon who specializes in urinary diversion. It is performed in a general hospital.
QUESTIONS TO ASK THE DOCTOR
- How soon after the surgery will I be taught how to use an ostomy?
- Will the ostomy be obvious to others?
- Is continent surgery, or surgery with an internal neo-bladder, a better alternative?
- How do conduit and continent surgery compare in terms of recuperation, complications, and quality-of-life issues?
She has been ill with a UTI and a urologist is recommending scoping the conduit because loops can develop that can allow pools of pus to form. He said that the conduit should be irrigated about twice a year.
We had not known about this at the time of the procedure to make the conduit which has functioned very well.
Dr Ellen Joyce
Any information would be helpful..thank you!
Another dr. suggests another resectioning of the baldder followed by chemo & radiation, he feels my fathers weight would strangle the part of the bowel that would have to come through the abdominal wall. Just with the info I have provided what are your thoughts. We actually have an appt. for a consulation with a dr. at hopkins but not until after the next resectioning is to be done and before chemo & radiation is to be started. As you can tell he is sort of leaning towards to dr. who suggested the resectioning again and chemo & radiation. How much of a factors is a persons weight when considering a ileal conduit? Thank you for any feed back you can offer.
Has anyone heard of it been reversed?
Any info would be great!
Thanks.
Hope this helps
Caroline Knight
Sir, my father had undergo through systectomy with ileal conduilt. but there comes pus in urine in very larg quantity.it comes when my father laughs or talk with forcfully. please tell me its a normal thing or its too dangerous.
if its abnormal, what medication should he use to recover himself.
i will be very thankful to your guidence.
Really, if another 2-3 inches of small bowel is taken to make a decent stoma - how will that impact on the client??? If anything, I believe it would be a good thing and take a great burden off of the clients affected. Thank you. Jane.
The bag is a two piece system. Also the bag she uses does not have clips, instead the bag adheres to the flange with a peel off adhesive, so it is softer more flexible than a clip, I believe.
Hope this helps as it was a huge solution to how we were doing the bag before. (We had to try to customize by cutting small pieces in pie shape pieces or using paste to fill in the gaps.) It was difficult and felt like each bag change was a procedure. It was also discouraging for my mother. Now so much easier & less stressful!
I am 78 and had the ileal surgery 2 months ago. Was in hospital 4 days, came home and was shoveling snow in about 2 weeks. While this is something to put up with,its not a big life changer.You can see pictures of the pouches at a number of sites. I get my supplies from Byram, you can see pictures of many different pouches at thir web site. I am using Convatec pouches, very thin and light. When full or almost full there is a slight bulge in the stomach area. Not too visible now because I am layered up with clothing in the cold weather we have been having. For patients with bladder cancer this is the most popular way to go. I still have my bladder but it was destroyed in a surgical accident 3 years ago.
When I replied to your post I ignored the fact that your father has bladder cancer. The ileal conduit is the most popular procedure for that, but removing the bladder means a longer more involved surgical procedure with longer hospitalization than simply the ileal conduit. Your father's choice is to go for the surgery or wait and see how long he can live with the bladder cancer. Tough choice.
The fact that it is not reversible it is my biggest fear. I am afraid she is going to have more infections and problems after the surgery. Is there anyone in So California that I can speak with? Because she is an independent adult I have no say over this decision.
The fact that it is not reversible it is my biggest fear. I am afraid she is going to have more infections and problems after the surgery. Is there anyone in So California that I can speak with? Because she is an independent adult I have no say over this decision.
But I now have stricture at the site of the illiam where it was rejoined after apiece was taken to make the stoma, this is causing dreadful constipation as the faecal matter has difficulties passing through the join to get to the bowel, this is gradually getting a lot worse causing abdominal pain. I am to have a colonoscopy soon soo hopefully I can get this sorted out once and for all.
Please be aware of the complications of this surgery. I would have never dreamed he would have fallen into to 10-12% range for complications
I’m just after some information if anyone can help?
My mum had bladder diversion with ileal conduit 9 weeks ago.
She hasn’t had any support which is really bad, just left the hospital and has pretty much dealt with everything on her own, other than 1 visit from a stoma nurse.
The question I could do with answering is how long before the brain realises the bladder is actually disconnected? It wasn’t removed and my mum had the operation as she had very severe IC , not cancer. It was a last resort thing having tried bladder stretches, injections, medications etc.
The thing is she can still feel her bladder like before. I’m just hoping this will improve as time goes on as she is extremely upset that the fullness and pressure feelings are there even though she has a stoma/bag.
She has an infection at the moment and I’m just wondering that is why the sensations are so bad? Any advice would be great, thanks in advance.