Endotracheal intubation
Definition
Endotracheal intubation is the placement of a tube into the trachea (windpipe) in order to maintain an open airway in patients who are unconscious or unable to breathe on their own. Oxygen, anesthetics, or other gaseous medications can be delivered through the tube.
Purpose
Specifically, endotracheal intubation is used for the following conditions:
- respiratory arrest
- respiratory failure
- airway obstruction
- need for prolonged ventilatory support
- Class III or IV hemorrhage with poor perfusion
- severe flail chest or pulmonary contusion
- multiple trauma, head injury and abnormal mental status
- inhalation injury with erythema/edema of the vocal cords
- protection from aspiration
Description
To begin the procedure, an anesthesiologist opens the patient's mouth by separating the lips and pulling on the upper jaw with the index finger. Holding a laryngoscope in the left hand, he or she inserts it into the mouth of the patient with the blade directed to the right tonsil. Once the right tonsil is reached, the laryngoscope is swept to the midline, keeping the tongue on the left to bring the epiglottis into view. The laryngoscope blade is then advanced until it reaches the angle between the base of the tongue and the epiglottis. Next, the laryngoscope is lifted upwards towards the chest and away from the nose to bring the vocal cords into view. Often an assistant has to press on the trachea to provide a direct view of the larynx. The anesthesiologist then takes the endotracheal tube, made of flexible plastic, in the right hand and starts inserting it through the mouth opening. The tube is inserted through the cords to the point that the cuff rests just below the cords. Finally, the cuff is inflated to provide a minimal leak when the bag is squeezed. Using a stethoscope , the anesthesiologist listens for breathing sounds to ensure correct placement of the tube.
Preparation
For endotracheal intubation, the patient is placed on the operating table lying on the back with a pillow under the head. The anesthesiologist wears gloves, a gown and goggles. General anesthesia is administered to the patient before starting intubation.
Risks
The anesthesiologist should evaluate and follow the patient for potential complications that may include edema; bleeding; tracheal and esophageal perforation; pneumothorax (collapsed lung); and aspiration. The patient should be advised of the potential signs and symptoms associated with life-threatening complications of airway problems. These signs and symptoms include but are not limited to sore throat, pain or swelling of the face and neck, chest pain, subcutaneous emphysema, and difficulty swallowing.
Normal results
The endotracheal tube inserted during the procedure maintains an open passage through the upper airway and allows air to pass freely to and from the lungs in order to ventilate them.
Alternatives
Alternatives to endotracheal intubation include:
-
Esophageal tracheal combitube (ETC). The ETC is a double-lumen tube,
combining the function of an esophageal obturator airway and a
conventional endotracheal airway. The esophageal lumen has an open upper
end, perforations at the pharyngeal level, and a closed distal end. The
tracheal lumen has open ends. The lumens are separated by a wall and
each is linked via a short tube with a connector. An oropharyngeal
balloon serves to seal the oral and nasal cavities after
insertion. At the lower end, a second cuff serves to seal either the trachea or esophagus.
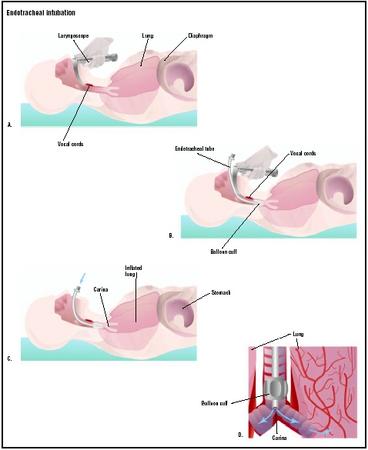 The doctor inserts the laryngoscope into the patient's mouth, advancing through the trachea to the vocal cords (A). An endotracheal tube is inserted into the airway (B). The balloon cuff is inflated, and the laryngoscope is removed (C). (Illustration by GGS Inc.)
The doctor inserts the laryngoscope into the patient's mouth, advancing through the trachea to the vocal cords (A). An endotracheal tube is inserted into the airway (B). The balloon cuff is inflated, and the laryngoscope is removed (C). (Illustration by GGS Inc.) - Laryngeal mask airway (LMA). The LMA consists of an inflatable silicone ring attached diagonally to a flexible tube. The ring forms an oval cushion that fills the space around and behind the larynx. It achieves a low-pressure seal between the tube and the trachea without insertion into the larynx.
- Tracheostomy. A tracheostomy is a surgically created opening in the neck that allows direct access to the trachea. It is kept open with a tracheostomy tube. A tracheostomy is performed when it is not possible to intubate the patient.
See also Anesthesia evaluation .
Resources
books
Finucane, B. T., and A. H. Santora. Principles of Airway Management. New York: Springer Verlag, 2003.
Roberts, J. T. Fundamentals of Tracheal Intubation. New York: Grune & Stratton, 1983.
Stewart, C. E. Advanced Airway Management. St. Louis: Quality Medical Publishing, 2002.
periodicals
Bochicchio, G. V., et al. "Endotracheal intubation in the field does not improve outcome in trauma patients who present without an acutely lethal traumatic brain injury." Journal of Trauma Injury, Infections and Critical Care 54 (February 2003): 307–311.
Erhan, E., et al. "Tracheal intubation without muscle relaxants: Remifentanil or alfentanil in combination with propofol." European Journal of Anaesthesiology 20 (January 2003): 37–43.
Udobi, K. F., E. Childs, and K. Touijer. "Acute respiratory distress syndrome." American Family Physician 67 (January 2003): 315–322.
Van de Leur, J. P., J. H. Zwaveling, B. G. Loef, and C. P. Van der Schans. "Endotracheal suctioning versus minimally invasive airway suctioning in intubated patients: A prospective randomized controlled trial." Intensive Care Medicine 186 (February 8, 2003).
organizations
American Society of Anesthesiologists. 520 N. Northwest Highway, Park Ridge, IL 60068-2573. (847) 825-5586. http://www.asahq.org/ .
other
"Endotracheal intubation." Health_encyclopedia. http://www.austin360.com/search/healthfd/shared/health/adam/ency/article/003449.html .
"Endotracheal intubation." PennHealth. http://www.penn health.com/ency/article/003449.htm .
"Intubation." Discovery_Health. <http://health.discovery.com/diseasesandcond/encyclopedia/1219.htmlgt; .
Monique Laberge, Ph.D.
Any info on this would be appreciated.