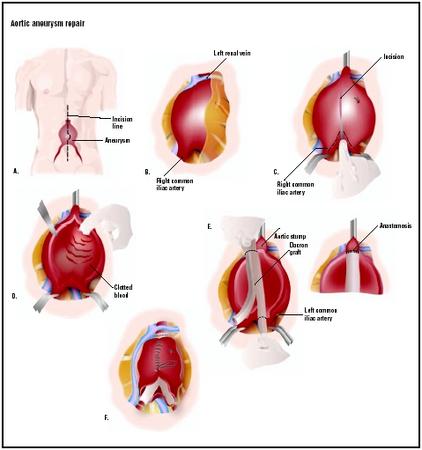
Aortic aneurysm repair
Definition
Aortic aneurysm repair involves the removal of a dilated (enlarged) portion of the aorta replaced by a woven or knitted Dacron graft to continue uninterrupted blood flow through the aorta and all branch vessels.
Purpose
Aortic aneurysm repair is performed when a portion of the aorta has become dilated as a result of medionecrosis in the ascending aorta or atherosclerosis in the arch and descending segments. Congenital defects in connective tissue are also a risk factor. A history of blunt trauma may be associated with this disease propagation. Prior to 1950, patients exposed to syphilis were at risk of developing aortic aneurysm. Risk of clot formation and rupture of the aneurysm, seen in 50% of cases, as well as dilation to a size greater than 4 in (10 cm) promote repair of the aneurysm by surgical techniques.
Demographics
The patient population for this procedure is typically male with an average age of 65 and a history of medionecrosis or atherosclerosis of the aorta. Patients with a medical history significant for syphilis or blunt trauma are at risk. Congenital defects associated with Marfan syndrome or Ehlers-Danlos syndrome (congenital tissue disorders) need to be monitored.
All patients will be monitored until the aneurysm demonstrates consistent enlargement over time, or grows to greater than 2.2 in (5.5 cm) in diameter at which time surgery is suggested. At a diameter of 4 in (10 cm) surgery is the best option, as risk of rupture increases. Many patients live without symptoms, having the aneurysm identified during other medical procedures.
Description
After general anesthesia is administered, the surgeon will make an incision through the length of the sternum to repair an ascending, arch, or thoracic aortic aneurysm. Abdominal aneurysms are approached through a vertical incision in the abdominal wall. Depending on the location of the aneurysm, cardiopulmonary bypass with deep hypothermic circulatory arrest (arch), cardiopulmonary bypass (ascending), or left heart bypass (thoracic) may be required. All procedures require some amount of anticoagulation, usually heparin, to be administered to prevent blood clot formation. Clamps will be applied across the aorta to prevent blood flow into the aneurysm. The aneurysm will be opened to an area where the tissue is healthy. The healthy tissue will be sutured to a synthetic fiber fabric graft. The fabric is knit or woven Dacron fibers and may be impregnated with collagen, gelatin, or other substances. Blood flow is reinstituted to check for a secure seal. Additional sutures will be added to prevent leaking. The incision is then closed at the completion of the procedure with blood drains penetrating the incision during healing.
Ascending aortic aneurysms may involve the aortic valve or coronary arteries. If the aortic valve is damaged, a graft with an integral aortic valve is used. The coronary arteries are reconnected to the graft.
Aortic arch aneurysms require the reattachment of the arch vessels, the innominate artery, the left common carotid artery, and the left subclavian artery. To decrease surgery time, these three vessels can be treated as a single vessel by using part of the patient's native aorta to create an island. This island is then connected to the graft.
Thoracic aneurysms require special care to protect the spinal vessels that supply blood to the spinal cord. Protecting the spinal cord during repair is still an area of intensive research. Some surgeons feel that rapid implant of the graft to restore blood flow is the best method to protect the spinal cord. A bypass graft called a Gott shunt can be used to redirect the blood flow around the area during surgical repair. Left-heart bypass provides the same benefit as a Gott shunt, with the addition of a mechanical pump for more controlled blood flow to the abdomen and lower extremities.
The abdominal aortic aneurysm is repaired by rapid anastomosis of the graft to return blood flow to the circulation. If the renal arteries are involved in the aneurysm, they will be reattached to the graft. Additionally, if the superior celiac, mesenteric, or inferior celiac arteries are involved, they will also be reattached to the graft. Finally, it is common for the bifurcation (separation into two) of the iliac arteries to be involved; this may require a Y-shaped graft to be used to reattach both lower limb vessels.
Diagnosis/Preparation
A simple x ray may provide the initial diagnosis of aortic aneurysm. Initial diagnosis can be made with non-invasive transesophageal echocardiography or ultrasound. Additional tests such as magnetic resonance imaging (MRI) or computed tomography (CT) will allow for additional visualization of the aneurysm. An angiography is the preferred method for determining the severity. Blood vessel and aortic valve health can be evaluated.
Aftercare
Following surgery the patient will be cared for in an intensive care unit . Cardiac monitoring will be continued for blood pressure and heart function. Intravenous fluids will continue to be given, and may include blood products. Additional medications will be continued to support cardiac function as needed. The ventilator will be removed after the patient is able to breathe on his/her own. The stay in the intensive care unit is approximately two to five days with hospital discharge following a week.
Risks
There are risks associated with general anesthesia, not associated with the aortic aneurysm repair. Additional risks of cardiopulmonary bypass are not associated with surgical repair. Depending on the type of aneurysm involved, the risks can differ significantly. Since blood flow to the spinal cord is jeopardized by the surgical repair, thoracic aorta aneurysm repair carries a relatively high rate of paralysis. Ascending arch aneurysms may jeopardize coronary blood flow and aortic valve function. Infection of the sternum can influence recovery time. Renal function can be impacted by abdominal aortic aneurysm repair. Renal function may improve or remain compromised. Long-term complications associated with the abdominal surgery include intra-abdominal adhesions, small bowel obstructions, and incisional hernia. Aortic arch aneurysms carry a risk of brain damage associated with deep hypothermic circulatory arrest.
Normal results
Repair of the aneurysm will provide normal blood flow to the systemic circulation. Pain associated with the aneurysm will be relieved by the repair. The risk of aneurysm rupture will be eliminated.
Morbidity and mortality rates
During 1999 over 15,000 deaths in the United States were attributed to aortic aneurysm as reported by the American Heart Association. Without treatment, the five-year survival rate is 13%. The Multicentre Aneurysm Screening Group studied non-emergent abdominal aortic aneurysm repair, showing a 2–6% mortality rate at 30 days post surgery. Emergency surgeries demonstrate 37% mortality. In another study, treatment of cardiac disease by open heart surgery, not cardiac catheterization intervention, demonstrated a better outcome prior to elective treatment for abdominal aortic aneurysm.
During treatment of thoracic aneurysm repair the incidence of paraplegia is 6–10%. Left vocal cord paralysis is recognized if the laryngeal nerve has been compromised by the procedure. Multiple organ failure is incident in death, with respiratory failure being among the most common. If the aneurysm is above or involves the renal arteries, renal failure can occur in 4–9% of patients.
Treatment of the ascending aorta and aortic arch repair carry many of the risks associated with cardiopulmonary bypass, including hemostatic difficulties, left ventricle dysfunction, or myocardial (heart muscle) dysfunction. Irreversible brain damage is also an additional risk.
Cardiac function can be compromised in all patients with thoracic or abdominal aortic aneurysms. Hemorrhage is of frequent concern and is more of a risk as the number of suture lines increases. Forty to seventy percent of all deaths can be contributed to cardiac malfunction and blood loss.
Alternatives
Endovascular graft placement is being used as a suitable option to the open surgical procedure. The endovascular graft can be placed using minimally invasive techniques that reduce or eliminate the stay in the intensive care unit. Light sedation and epidural anesthetic are often adequate.
Resources
books
Hensley, Frederick A., Donald E. Martin, Glenn P. Gravlee, eds. A Practical Approach to Cardiac Anesthesia. 3rd Edition. Philadelphia: Lippincott Williams & Wilkins Philadelphia, 2003.
periodicals
Busch, T., et al. "Importance of Cardiovascular Interventions Before Surgery for Abdominal Aortic Aneurysms." Cardiovascular Surgery 18 (2000):18–21.
Cooley, D. "Aortic Aneurysm Operations: Past, Present, and Future." Ann Thorac Surg 67 (1999):1959–62.
"The Multicentre Aneurysm Screening Study (MASS) into the Effect of Abdominal Aortic Aneurysm Screening on Mortality in Men: A Randomized Controlled Trial." The Lancet 360 (November 2002):1531–1539.
Porter J. M., et al. "Endovascular Aortic Grafting: Current Status." Cardiovascular Surgery 7 (1999):684–691.
other
American Heart Association. 2002 Heart and Stroke Statistical Update. Dallas, TX: American Heart Association, 2001.
Allison Joan Spiwak, MSBME
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED?
Cardiothoracic or cardiovascular surgeons or vascular surgeons can perform these procedures. Abdominal and thoracic aortic aneurysm repairs require less sophisticated equipment during the surgical procedure, but do need extensive intensive care post-operatively. Anesthetic management plays a crucial role in the decrease in complications associated with these procedures. Facilities that can also provide cardiovascular surgery are best equipped to manage these patients, but this is not a limitation for all procedures.
QUESTIONS TO ASK THE DOCTOR
- How many of these procedures have been performed by the surgeon?
- What is the mortality rate for this procedure at the institution?
- What side effects are associated with this surgical procedure, and at what rate are they experienced by patients?
- What is the expected length of stay in the hospital?
- Are there any other suitable procedures, such as endovascular grafting?
- How long before normal activities, exercise, work, and driving can be resumed?
My Gramps who's about to turn 81 has been diagnosed with AAA.
Now I'm not sure about the measurements but he mentioned something about 14cm. From what I have read I would have thought that the Aorta would have split. Anyway about 5 years ago he had a tripple bypass done and with this the Cardio docs are concerned that his heart is not strong enough to make it through the op - they give him a 50/50 chance. Taking this into consideration and if the size of the AAA is right would it not be in his interest to undergo the op, can surgeons really refuse to do an op on someone with a 50/50 chance? I always thougth that the medical profession is there to try their damndest to help, irelevant of the odds....
http://www.insideheart.com/
could anybody explain this surgery in detail, the prefered machines, their benefits, the difference and function of this eqippment.
Our family still have this guilt, and believe proper equippment were not used.
Please help us to know the facts.
Thanks,
God Bless.
1) During surgery, will the blood flow be diverted even though the renal arteries are involved ( the TAA is anterior and posterior to the renal arteries).
2) Or will the cellular replacement cardiac machine be utilized?
3) After recovery, will there be decreased preexisting femur head,leg pain and old post surgical laminectomy pain, as well as less fatigue?
4)When the graft includes the healthy renal arteries, will blood flow improve in them?
Thanks All for your inputs and experiences into open TAA surgery in advance. I want to know everything I can about it presurgery.
She was in ICU for 2 weeks and intubated during this time.
She was transferred to med/surg and and another chest tube has been placed and still in. They say there is still fluid around the lungs. They say say there is 10cc of fluid in the chest tube per shift. They say it is old blood. She has back pain and taking Tylenol. Something does does seem write about this surgery and everything she has gone thru. They did a CT weeks ago and said they did not see any leak from the graft.
Very concerned and wondering if it is a leaky graft.